Page 2 :
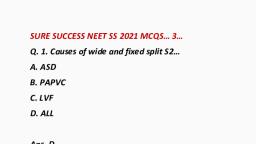
Ostium primum……. 10% of ASD. Due to persistence, of Ostium primum. Associated with AVSD., Sinus venosus………… 2 to 10% of ASD. Associated, with partial anomalous pulmonary venous return, (PAPVR)., Located in posterior atrial septum., Coronary sinus………. 1 to 2% of ASD. Due to, complete or partial unroofing of coronary sinus, onto posterior wall of LA., PATHOPHYSIOLOGY, Magnitude of shunt depends on size of defect and, compliance of ventricle., LV less compliant., Left to right shunt., Volume overload of RV., Impaired systolic and diastolic RV function., Increased pulmonary blood flow., Pulmonary hypertension in early adulthood., Eisenmenger syndrome…. R to L shunt.
Page 3 :
ASD<6 mm in diameter usually regress during first, year of life., Defects>8 mm in diameter usually enlarge., Clinical presentation…, Asymptomatic, Clinical symptoms usually apparent when, Qp:Qs>2:1., Reduced exercise capacity, Recurrent respiratory infection, Palpitation, Atrial fibrillation, CHF, Cyanosis (Eisenmenger syndrome), Prominent RV impulse, Leftward displacement of apex, Systolic flow murmur on left upper sternal, border(increased flow through pulmonary valve), Wide fixed split S2
Page 4 :
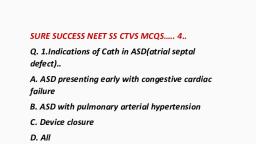
Apical middiastolic murmur (flow through tricuspid, valve), Diagnosis, ECG.. RV hypertrophy with prominent R wave., Right axis deviation, atrial fibrillation., CXR.. Cardiomegaly and prominent lung markings., Echocardiography… modality of choice… bubble, contrast from agitated saline injection., MRI and CT…, Cardiac catheterization….. A step up in oxygen, saturation can be observed from SVC to RA., Indications of treatment, Qp:Qs>1.5:1, Closure is performed between 2 to 5 years of age., In adult ASD associated with RV volume overload,, arrhythmia and heart failure., PVR>8 to 12 wood unit/m2 is contraindicated to, surgery., Treatment….
Page 5 :
Catheter based device can be used to close ASD, upto 3.8 cm in size., ASD with larger size, small septal rim or associated, PAPVR are not candidate for catheter based, closure., Malposition or embolization is complication., Surgical closure, Warden procedure, Complications, Patch dehiscence, Heart block, Sinus node dysfunction Atrial fibrillation, Residual shunt, , END OF ASD……………
Page 6 :
COR TRIATRIATUM, Cor triatriatum sinistrum is a separation of LA into, 2 chambers by a fibromuscular membrane., A Common pulmonary venous chamber and a, chamber containing the LA appendage and the, mitral valve., The communication between both chambers is, limited to one or multiple perforation on the, membrane., Sign and symptoms, Pulmonary venous Congestion, Poor growth, Pulmonary oedema, Pulmonary infection, Pulmonary hypertension, RHF
Page 8 :
VENTRICULAR SEPTAL DEFECTS…., A VSD is an abnormal opening between RV and LV., A VSD develops from congenital malformations,, trauma or MI., ANATOMY, The membranous septum is a fibrous structure, located below the septal leaflets of tricuspid valve., Inlet VSD are often associated with mitral valve, defects., The outlet is located below the pulmonic valve and, superior to the crista supraventricularis., The muscular septum is located along the, trabecular septum., TYPES, Membranous… membranous septum defect is, located below septal leaflets of tricuspid valve.
Page 10 :
Right to left shunt., Cyanosis., INFANTS, Congenital VSD are the most common congenital, lesion., They are found 2 out of every 1000 births., VSD are most commonly associated with tetralogy, of fallot, PDA and aortic coaractation., Harsh Pansystolic murmur common in VSD., Symptomatic patients develop growth failure,, tachypnea and Hepatomegaly., Most VSD will close spontaneously., 30% of infants will require surgery due to, development of heart failure during first year of, life., Outlet and inlet VSD unlikely to close, spontaneously.
Page 11 :
All symptomatic membranous and muscular VSD, should be repaired surgically regardless of age if, medical management fails., Asymptomatic membranous and muscular VSD, should be followed with serial Echocardiography., Indications of surgery are…, Increased PVR, Increased PA pressure, Symptoms, A PVR> 8 wood units /m2 that does not decrease, with Inhaled nitric oxide or 100% oxygen is, contraindicated to surgery., TREATMENT, Result of surgical repair are excellent., Right bundle branch block is common after VSD, repair., Residual VSD tend to close spontaneously., ADULT, Congenital, traumatic or post ischemic.
Page 12 :
Adult VSD is Restrictive., Indications of repair include Qp:Qs> 1.5 with or, without symptoms., Contraindications to repair PVR> 6 wood units/m2., , END OF VENTRICULAR SEPTAL DEFECTS…
Page 13 :
ATRIOVENTRICULAR SEPTAL DEFECTS, Atrioventricular septal defect is also called as AV, canal defect., A partial canal defect is just an Ostium primum, ASD, typically with a complete cleft of the Al of the, mitral valve., There may be gooseneck deformity of the LVOT,, which is an elongation of LVOT owing to apical, displacement of AVV plane., A complete AV canal defect(CAVC) consist of, primum ASD and unrestrictive inlet VSD and a, common AVV., There are three types of CAVC…, Rastelli A…. 75%...Defined by complete deviation, of superior common leaflet over the septal crest., VSD is often small., Rastelli B… Rare and almost never seen with, balanced ventricle. Straddling chord extends from
Page 14 :
the TV component into the LV or from the MV, component into the RV., Rastelli C…. 25%...There is an undivided superior, common leaflet usually without any chordal, attachment of the central part of the leaflet to the, septum. Most often associated with tetralogy of, fallot., In AV canal defect, both the coronary sinus and AV, node are Displaced inferiorly.The bundle of His, travels in the crest of the interventricular septum., The most important associated noncardiac, anomaly is Down syndrome., PATHOPHYSIOLOGY AND CLINICAL PRESENTATION, Left to right shunting with resultant increased, pulmonary blood flow and the AVV regurgitation., Therefore medical therapy consists of, anticongestive measures and afterload reduction if, AVV insufficiency is significant., CAVC have large left to right shunt.
Page 15 :
Elevated RV and PA pressure owing to unrestrictive, VSD., They present early within 4 to 6 weeks with, symptoms of pulmonary hypertension and, CHF(difficulty feeding, tachypnea and failure to, thrive)., CHF symptoms are more pronounced and, presentation is earlier when MV insufficiency, LV, underdevelopment or LVOTO are present., These lesion will result in the development of, pulmonary vascular occlusive disease if not, repaired in infancy., In Down syndrome, there is pronounced tendency, towards accelerated pulmonary vascular disease, when pulmonary hypertension is present., Diagnosis…., CXR.. Increased pulmonary blood flow.. Dilatation, of cardiac chambers, Echocardiography… diagnostic., Cardiac catheterization… gooseneck deformity.
Page 16 :
Treatment…, Surgical.., Timing of surgery… 1 to 2 years of age in partial, canal defect., CAVC defect should be repaired at 2 to 4 month of, age., , END OF ATRIOVENTRICULAR CANAL DEFECTS…..
Page 17 :
INTERRUPTED AORTIC ARCH….., Interrupted aortic arch is a rare defect, comprising, 1% of all congenital heart defects., It is absence of continuity between the ascending, and descending aorta., Typically a VSD is present in 80% of cases…, PATHOPHYSIOLOGY, Type A…. Distal to left subclavian artery (30%)., Type B…. Between the left subclavian artery and, the left common carotid artery (65%)., Type C… Between the left carotid and, brachiocephalic artery., Untreated, the median survival is 4 days., CLINICAL PRESENTATION….., Metabolic acidosis, Hemodynamic collapse with the closure of PDA., CHF
Page 18 :
DIAGNOSIS, Echocardiography, TREATMENT, IV PGE1 infusion can keep the ductus open and, correct the acidosis., Mechanical ventilation, Inotropic support, Treatment is surgical, Aortic arch reconstruction by direct anastomosis or, patch aortoplasty., Closure of VSD., Mortality is 30%.
Page 19 :
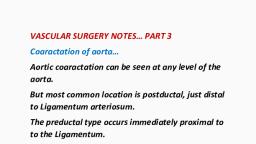
END OF INTERRUPTED AORTIC ARCH….., COARCTATION OF AORTA…., PATHOPHYSIOLOGY, Coarctation of aorta is hemodynamically, significant narrowing of aorta, usually present just, proximal to site of insertion of the ductus, arteriosus, distal to left subclavian artery., Narrowing of lumen., Associated lesion include Bicuspid aortic valve (50, to 80 %), VSD(30 to 60 %)., Compensatory collaterals are characteristics in, children and adolescent., The internal mammary arteries, posterior, intercostal arteries and anterior spinal arteries can, be dilated., Both systolic and diastolic pressures are elevated, above the coaractation.
Page 20 :
Below the coaractation, the systolic pressure is, lower than that of upper extremities but the, diastolic pressure tend to be normal., Aortic coaraction represents 4 %of congenital, heart lesion., Male to female ratio is about 3 :1., Associated with Turner’s syndrome., CLINICAL PRESENTATION, Clinical presentation and timing depends on the, degree of coaractation., 50% of patients present in first month of life with, signs of CHF, Dyspnea, distal organ malperfusion,, absent femoral pulse and Metabolic acidosis as the, ductus starts to close., Older children with milder form of disease may, present with irritability, failure to thrive,, diaphoresis and poor feeding., Adult may present with unexplained hypertension,, lower extremity claudication.
Page 21 :
Without intervention, severe hypertension, heart, failure, aortic rupture or stroke can develop., The mean age of survival for untreated disease is, less than 20 years., DIAGNOSIS, Physical examination… gallop rhythm with systolic, and diastolic murmur, prominent carotid pulsation,, diminished or absent femoral pulse, differential in, arterial pressure and oxygen saturation between, upper and lower extremities., CXR…. Cardiomegaly, rib notching in chronic cases, due to erosion of ribs by hypertensive intercostal, arteries., Chest radiograph of woman with Unrepaired, coaractation demonstrating rib notching from, dilated and tourtous intercostal arteries is shown, below……
Page 26 :
TREATMENT, IV PGE1 infusion can keep the ductus open and, provide perfusion to descending aorta in neonate., Inotropic support., Balloon angioplasty…. Carries significant, restenosis rate(75%)., Used for treatment of critically ill neonates that, are poor surgical candidate or for relief of, recurrent coaractation following repair., Surgical intervention is indicated in symptomatic, neonates, infants and adults., Left posterolateral thoracotomy approach is used., Direct end to end anastomosis.., Coaractation resection and end to end, anastomosis. The circumferential anastomosis is, completed with Interrupted sutures anteriorly.