Page 1 : Atrial Septal Defect, Check for, undaten, Elisa A. Bradley, MD2, *, Ali N. Zaidi, MDb, KEYWORDS, • Atrial septal defect • Congenital heart disease • Pulmonary arterial hypertension, • Ostium secundum defect • Ostium primum defect • Sinus venosus defect, KEY POINTS, • Atrial septal defects are among the most common types of congenital heart disease that may go, undiagnosed in childhood and may initially be found in adulthood., • Adults with an atrial septal defect are often asymptomatic, but may present with nonspecific symp-, toms such as dyspnea on exertion or exercise intolerance., • Pulmonary arterial hypertension and atrial arrhythmias may develop as a consequence of a long-, standing unrepaired atrial septal defect., Management of the adult with an atrial septal defect must include consideration of whether or not, pulmonary arterial hypertension is present, degree of shunting, and anatomy., • Therapeutic considerations for an unrepaired atrial septal defect in the adult include pulmonary, arterial vasodilator therapy, interatrial septal rim assessment, and candidacy for percutaneous, versus surgical repair., Video content accompanies this article at http://www.cardiology.theclinics.com., evaluation by specialized and experienced pro-, vides in the field of adult CHD.2, The purpose of this review is to describe ASD, anatomy and various physiologic presentations in, the adult. The goal is to review common clinical, presentations and findings on imaging and special, testing, and to discuss both practical and, advanced management strategies inclusive of, medical therapeutic considerations, surgical, repair options, and percutaneous closure., INTRODUCTION, Atrial septal defects (ASD) are considered one of, the most common congenital heart defects, (CHD) found in the adu, lence of ASDS in adults is 0.88 per 1000 patients.", Frequently, the reason that this lesion is not, detected sooner is that many patients are asymp-, tomatic until the second to fourth decades of life, a, time after which increased pulmonary blood flow, may lead to pulmonary vascular remodeling and, ultimately affect shunt direction and end-organ, perfusion. Although this lesion is classified as a, simple form of CHD, complex physiologic changes, related to pulmonary vascular remodeling and, shunt direction often complicate the presentation., Therefore, the assessment and treatment options, vary widely between patients and require, The estimated preva-, ANATOMY AND PHYSIOLOGY, Anatomy, There are 4 main types of defects that occur in the, atrial septum and lead to the formation of an ASD, (Fig. 1).2 The most common type of ASD is the, ostium secundum defect, which accounts for, a Department of Internal Medicine, Division of Cardiovascular Medicine, The Ohio State University, Columbus,, OH, USA; Mount Sinai Cardiovascular Institute, The Children's Heart Center, Kravis Children's Hospital, lcahn, School of Medicine at Mount Sinai, 1 Gustave L. Levy Place, 1190 5th Avenue, Box 1030, New York, NY, 10029, USA, * Corresponding author. Davis Heart Lung Research Institute, 473 West 12thAvenue, Columbus, OH 43210., E-mail addresses:
[email protected];
[email protected], Twitter: @drelisabradley (E.A.B.); @AliZaidi MD (A.N.Z.), Cardiol Clin 38 (2020) 317-324, https://doi.org/10.1016/j.ccl.2020.04.001, 0733-8651/20/© 2020 Elsevier Inc. All rights reserved., Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on December 29, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved., cardiology.theclinics.com
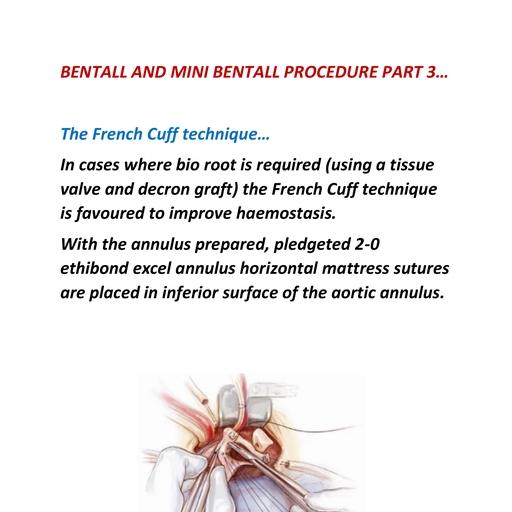
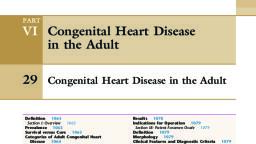
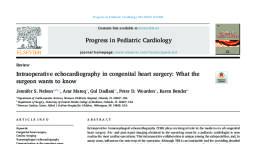
Page 2 : 318, Bradley & Zaidi, (APressure = Flow x Resistance, AP = QR). So, long as flow and resistance are low, the degree, of shunting that occurs is based on end-, diastolic filling pressures, compliance, and the, anatomy and size of the defect. This lesion is, generally well-tolerated in children, adolescents,, and the young adult, in part owing to low filling, pressures in the heart and high compliance in a, system with normal pulmonary vascular resis-, tance (PVR). However, in the case of a sizable, ASD, over time the increased left-to-right flow, across the defect leads to enlargement of the, RA and right ventricle. This finding may be the, first clue to the presence of an ASD., Superior Vena Cava, Ostium, Secundum, defect, Superior sinus, venosus defect, Tricuspid Valve, Inferior sinus, venosus defect, Ostium, Abnormal Physiology, Primum, Coronary, In a minority of patients, the pulmonary overcircu-, lation that results from a septal defect may, abnormal pulmonary vascular, remodeling and elevation in PVR, culminating in, the development of pulmonary arterial hyperten-, sion (PAH). Up to 16% of adults who present, with an ASD have concomitant PAH. In most, cases, although pulmonary artery pressures are, elevated, they remain lower than the systemic, blood pressure. However, in a minority of cases,, the pulmonary vascular pressures increase to sys-, temic or suprasystemic levels, resulting in reversal, of the shunt (right-to-left flow) and peripheral, desaturation with cyanosis, a condition called, Eisenmenger syndrome. In general, therapeutic, options for the patient that has developed frank, Eisenmenger syndrome are limited in comparison, with the adult with an unrepaired ASD and mild, to moderate PAH. Recent studies have shown, defect, sinus, defect, Inferior Vena Cava, contribute to, Fig. 1. Anatomy of the interatrial septum and septal, defects. Anatomy of the interatrial septum demon-, strating the location(s) of the 4 main types of ASDS:, secundum, primum, sinus venosus, and coronary sinus,, as viewed from the RA., approximately 80% of ASDS. This defect arises, owing to a deficiency of tissue at the level of the, fossa ovalis. Ostium primum ASDS account for, about 10% of septal defects and develop owing, to a deficiency in tissue near the atrioventricular, valves. Ostium primum ASDS are associated with, a cleft in the left-sided atrioventricular valve and, are often more aptly referred to by the synony-, mous term, partial atrioventricular septal defect., Sinus venosus defects occur more commonly in, the superior (vs inferior) portion of the embryologic, sinus venosus and commonly occur with partial, anomalous pulmonary venous return, particularly, of the right upper pulmonary vein. Coronary sinus, defects, frequently referred to as unroofed coro-, nary sinus, are the least common type of ASD, and often are missed on traditional imaging modal-, ities. However, an unroofed coronary sinus may be, detected when agitated saline contrast bubbles, from the left upper extremity enter the left atrium, (LA) first, before the right atrium (RA)., that those patients with ASD and mild to moderate, PAH may respond favorably to PAH-specific med-, ical therapy, and potentially regress PVR to a level, at which septal defect repair may be possible, and, perhaps impact long-term morbidity and mortality, (Table 1)., CLINICAL PRESENTATION, Most adults who present with a newly diagnosed, unrepaired ASD are asymptomatic, and the finding, is incidental. However, in a minority of patients, a, careful medical history and clinical examination, may suggest the presence of an unrepaired ASD., In these patients, the history often reveals a, gradual change in exercise capacity, commonly, reported as subtle, and occasionally overt, dys-, pnea on exertion. Typically, a patient may describe, this change occurring over the preceding months, to years; however, if PAH is present, this change, can occur more abruptly, on the order of weeks, to months. Less frequently, palpitations may, Normal Physiology, When resting cardiopulmonary hemodynamics, are normal in the presence of an ASD, blood, shunts from the oxygenated LA through the ASD, to the deoxygenated blood pool in the RA,, creating a step-up in oxygen saturation at the, level of the RA. Hemodynamics in the setting of, an ASD are governed by Ohm's law as it relates, to fluid flow in the pulmonary vascular bed, Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on December 29, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
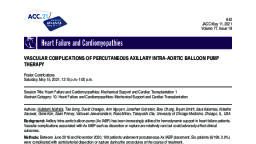
Page 3 : Atrial Septal Defect, 319, Table 1, Studies evaluating delayed ASD closure in moderate to severe PAH, Author, Year, Timeframe, Location, Therapy, Outcomes, Cho et al, 17, 2011, PDE5I, ERA,, Inh Prost, 2004-2009, Korea, 16, All closed with fenestration, (PVR od 9.8), Fujino et al,, 2015, 12, 2013, Japan, ERA, Inh Prost, 1 patient had preclosure, treatment, Bradley et al, 13, 2013, 5 (33%) underwent closure, PVR of 8.8 (7.2 → 4.6, vs 9.9 → 8.2), 1998-2012, U.S., 15, PDE5I, ERA,, Prost, Kijima et al, 14, 2016, 8 (22), PDE5İ, ERA,, Inh Prost, 2006-2014, Japan, All received closure, (PVR 9.6 → 4.0), 7 (17), 15, Song et al,, 2016, PDE5İ, ERA,, Inh Prost, 2001-2012, Korea, All closed with fenestration, (PVR 9.2 → 6.3), Bradley et al, 16, 2018, 1996-2017, US, 69, PDE5I, ERA, PC, 19 (28%) underwent closure,, closure group: ↑ RV, function, ↑ 6MWTD,, trend ↑ survival., Abbreviations: 6MWTD, 6-minute walk test distance; ERA, endothelin receptor antagonist; Inh, inhaled; PC, prostacyclin;, PDE5İ, phosphodiesterase type 5 inhibitor; RV, right ventricle., evaluate the size of the RA and right ventricle,, which are typically enlarged. This study can also, provide information about pulmonary artery pres-, sure, and may be the first clue as to the presence, of PAH. In the patient with good transthoracic, echocardiogram image quality, the interatrial, septum can be visualized and color Doppler inter-, rogation may be used to determine if a defect is, present. Agitated saline contrast is often adminis-, tered to determine if there is a septal defect pre-, sent and, in the case of an ASD, demonstrates, extravasation of saline contrast microbubbles, occur, especially in those that have developed an, occult atrial arrhythmia, which is more common in, the patient who presents at an older age. On phys-, ical examination, there may be a soft systolic, crescendo-decrescendo outflow tract murmur, owing to increased flow across the pulmonary, valve, accompanied by a fixed split in the S2 heart, sound owing to delayed closure of the pulmonic, valve., INVESTIGATION AND ASSESSMENT, Often the first test that a new patient with dyspnea, receives is an electrocardiogram. This test can be, helpful if an ASD is suspected, because these pa-, tients commonly demonstrate an incomplete right, bundle branch block. More specifically, in the, presence of a secundum ASD right axis deviation, and crochetage (crochet-like hook) of the inferior, lead R waves may be seen. In primum ASD,, incomplete right bundle branch block is more likely, to occur in the presence of left axis deviation. If a, chest radiograph is sought, it is often normal., However, if the patient has developed PAH, there, may be cardiomegaly and increased pulmonary, vascularity., Ultimately, imaging is required to confirm the, diagnosis of an ASD. Frequently, a transthoracic, echocardiogram is the preferred initial imaging, test. The limitation of the transthoracic echocar-, from the RA to the LA at the level of the interatrial, septum., In most cases, a transesophageal echocardio-, gram (TEE) is required to more closely examine, the interatrial septum to determine both the type, and size of the ASD. These factors become impor-, tant when considering therapeutic options with, respect to closure and repair of the defect. Typi-, cally, the interatrial septum and defect are imaged, in at least 3 different TEE planes: 0° and 90° at the, mid esophagus, and 30° at the high esophageal, level (Fig. 2, Videos 1-3). Although these views, provide an adequate evaluation of the interatrial, septum and rims, the inferior vena caval rim is, often not well-visualized on TEE and, if it is sus-, pected to be deficient, may require intravascular, echocardiography at the time of hemodynamic, evaluation., diogram is that it may be impacted by poor acous-, tic windows related to the adult body habitus., However, image quality is often sufficient to, Although advanced cardiac imaging such as, computed tomography and cardiac MRI are not, required to make the diagnosis of an ASD, these, Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on December 29, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 4 : 320, Bradley & Zaidi, A, Superior, В, O Degrees, Left atrium, Postero-, Antero-, Anterior-, superior, Superior, inferior rim, rim, Posterior-, Superior, Right atrium, Anterior-, Inferior, Posterior-, Inferior, 7.0C, 37.1C, 30 Degrees, 0 Degrees, Inferior, C, 30 Degrees, 90 Degrees, Left atrium, Left atrium, Postero-inferior rim, Superior rim, Inferior rim, Antero-superior rim, Right atrium, Right atrium, 37.0C, 38.8C, Fig. 2. Transesophageal imaging planes of the interatrial septum. Imaging planes of the interatrial septum (A), when evaluated by TEE include mid esophageal views at 0° (B) demonstrating the posterosuperior and anteroin-, ferior rims and at 90° show the superior and inferior rims (D). High esophageal views at 30° (C) are required to, demonstrate the posteroinferior and anteroinferior rims., tests may be completed during the clinical, workup. Advanced imaging provides high quality, data on chamber size and function and can be, helpful in determining whether or not anomalous, pulmonary venous return is present, particularly, when the pulmonary veins are not fully evaluated, on TEE (Fig. 3). Additionally, flow quantification, on cardiac MRI may be used to evaluate Qp:Qs, in the presence of a septal defect., Invasive hemodynamic right heart catheteriza-, tion (RHC) is usually one of the last tests to be, completed in the presence of an ASD, particularly, when defect repair is being considered. RHC al-, lows for the evaluation of shunt flow and in partic-, ular is helpful in quantifying the degree and, direction of shunting. Intravascular echocardiogra-, phy is frequently undertaken during RHC if TEE im-, ages are inadequate in evaluation of the defect,, and if or when percutaneous closure is being, considered. Intravascular echo is often used to, provide direct visualization of the interatrial, septum and allows for real-time 2-dimensional im-, aging guidance at the time of percutaneous, closure., Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on December 29, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 5 : Atrial Septal Defect, 321, B, Fig. 3. Cardiac MRI evaluation for ASDS. Routine cardiac MRI sequences used to define the atrial septum on, bright blood images (gradient echo sequences) (A) and dark blood images (fast spin echo sequences) (B). These, images allow definition of atrial septal anatomy (red arrow, secundum ASD), atrial and ventricular morphology, and are used to assess volumetric data and to quantify ventricular function. High spatial resolution MR angiog-, raphy with 3-dimentional volume rendered imaging is used to define cardiac anatomy and morphology of the, great vessels and systemic and/or pulmonary veins (C). The double red arrows demonstrate anomalous return, of right-sided pulmonary veins to the superior vena cava., Finally, exercise testing may be done before or, after RHC in select cases. This testing can be, accomplished in the form of a 6-minute walk test, or more formal cardiopulmonary exercise testing., The purpose of exercise testing is not only to eval-, uate objective exercise tolerance, but also to, assess oxygenation at rest and with peak exer-, cise. In patients with normal resting hemody-, namics (and in the absence of significant lung, disease), oxygen saturation is typically normal., However, with exercise, a minority of patients, demonstrate significant increases in the PVR., This hemodynamic change can cause a previous, left-to-right or minimally bidirectional shunt to, become right-to-left with activity, and results in, exercise-induced desaturation. In this situation,, closure of the defect may be unsafe and often, PAH-specific medical therapy may be considered,, even when resting pulmonary artery pressures, may be normal (see Table 1)., shunts, a Qp:Qs of >1.5 and evidence of right, heart volume overload in the absence of signifi-, cant PAH) typically benefit from surgical, catheter closure of the ASD." Asymptomatic, patients with a significant left-to-right shunt, (Qp:Qs of >1.5) and evidence of right heart, enlargement also benefit from closure, because, continued overcirculation in an already dilated, right heart increases the likelihood of late clinical, complications, including decreased functional, capacity, atrial arrhythmia, and the development, of PAH.5,6, trans-, Contraindications for Repair, Closure of an ASD is not recommended in pa-, tients with a clinically significant right-to-left, shunt and those with severe PAH (PVR of >8, Wood units or irreversible pulmonary vascular, occlusive disease, desaturated at rest). There, are emerging data that support that patients, with a pulmonary artery pressure of less than, two-thirds of the systemic arterial pressure, a, PVR of less than two-thirds of the systemic resis-, tance, or a positive response to pulmonary vaso-, dilator testing may be considered for ASD, closure.® A fenestrated device is often considered, MEDICAL DECISION MAKING AND, THERAPEUTIC CONSIDERATIONS, Indications for Repair, Small ASDS may spontaneously close in child-, hood; however, larger defects may contribute, to hemodynamic abnormalities and clinical, symptoms if left unrepaired. The decision to, repair an ASD is based on clinical and anatomic, information, including the size and location of the, defect, magnitude of hemodynamic impact of, the shunt, and the presence and degree of, PAH, if present. Patients with decreased func-, tional capacity caused by hemodynamically sig-, nificant ASD's (moderate or large left-to-right, in these cases to ensure that an adequate "pop-, off" is present so that if RA pressure rises above, the LA pressure, cardiac output is conserved., Relative contraindications to closure typically, are regarded for percutaneous cases and, include: defects larger than 36 mm, inadequate, margins and rims to safely anchor the device,, and/or interference of the device with the atrio-, ventricular valves or venous drainage., 7., Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on December 29, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.