Page 1 : 13, Congenital Heart Disease:, General Principles and Imaging, Michael A. Quail, Andrew M. Taylor, , CHAPTER OUTLINE, Introduction, 289, Clinical Presentation, 289, Morphological Description and Sequential Segmental, Analysis, 290, Physiological and Functional Assessment, 292, Non-Invasive Imaging Techniques, 292, , INTRODUCTION, Although rare, with an incidence of 8 per 1000 births, congenital heart, disease (CHD) has increased in prevalence due to the success of surgical, and medical management in childhood. A significant proportion of, patients with repaired CHD surviving to adulthood fall under the care, of cardiologists outside tertiary centres for congenital cardiac care., Specialist cardiovascular and general radiologists require an understanding of the underlying morphological abnormalities and their physiology,, methods of repair and how potential complications may be detected, and assessed in their practice, using appropriate imaging techniques,, such as echocardiography, magnetic resonance imaging (MRI), cardiac, magnetic resonance (CMR) and computed tomography (CT)., CHD is any developmental malformation of the heart. The spectrum, of disease falling into this classification ranges from simple lesions—for, example bicuspid aortic valve—through to more complex diseases, involving single ventricle lesions, such as hypoplastic left-heart syndrome., The underlying causes of CHD remain relatively poorly understood,, although the epidemiology suggests a genetic basis contributing to the, majority of CHD. Aneuploidies—for example, trisomy 21 (Down, syndrome, septal defects) and monosomy X (Turner syndrome, bicuspid, aortic valve and coarctation)—are the earliest identified causes and, account for 10%–20% of CHD. Copy number variations (small to large, deletions or duplications) lead to altered dosage of genes and may, represent another important mechanism; an example is Del22q11, which, causes DiGeorge syndrome (interrupted aortic arch, tetralogy of Fallot, (TOF), truncus arteriosus). Unfortunately, the cause of CHD in most, patients remains unknown., , CLINICAL PRESENTATION, The clinical presentation of CHD in infancy may be dominated by a, number of physiological states., 1. Left-to-Right Shunts: Redirection of blood from the systemic (left), to the pulmonary circulation (right) may occur at atrial, ventricular, or great vessel level. A proportion of already oxygenated blood is, , Specific Lesions, 296, Acyanotic Lesions, 296, Cyanotic Congenital Heart Disease, 304, Single Ventricles, 311, Conclusion, 313, , recirculated to the lungs with each heartbeat, resulting in inefficiency., The volume of the shunt and its location accounts for the observed, signs. Chambers and vessels receiving the excessive volume enlarge, and high pulmonary blood flow results in pulmonary plethora., Typical examples include atrial septal defects (ASDs), ventricular, septal defects (VSDs) and patent ductus arteriosus (PDA). Patients, are pink but increasingly breathless with larger shunts., 2. Compromised Systemic Perfusion: This may result from low stroke, volume of a systemic ventricle (hypoplastic left-heart syndrome),, outflow tract obstruction (critical aortic stenosis (AS)) or aortic, obstruction (interrupted aortic arch or coarctation). The clinical, picture is one of poor peripheral perfusion, with low-pulse volume;, patients may be pink or blue (cyanotic). The ductus arteriosus may, provide an effective temporary bypass for the obstruction, facilitating, systemic perfusion with deoxygenated or mixed blood; however, as, the duct closes (some days after birth), life-threatening systemic or, lower body hypoperfusion ensues and, often, pulmonary venous, hypertension. Therapy is directed at maintaining the patency of, the arterial duct using intravenous prostaglandins, intensive care, for critically ill patients and planning for surgical relief of the, obstruction., 3. Pulmonary Venous Congestion: Obstruction to pulmonary venous, return results in increased pulmonary venous pressure (elevated, pulmonary capillary wedge pressure); at progressively higher, transvascular gradients, oncotic pressure is exceeded and extravasation, of fluid into the interstitial and alveolar space occurs. Obstruction, may occur in the pulmonary venous pathway (total anomalous, pulmonary venous connection, TAPVD), in the atrium (cor triatriatum) or at the level of the left ventricle (LV) inflow (supravalvular,, valvular or subvalvular mitral stenosis or mitral regurgitation)., Pulmonary venous congestion may also occur as a function of elevated, left atrial pressure secondary to LV diastolic dysfunction; increased, LV end diastolic pressure (valve disease, aortic coarctation, myocardial, disease). The degree of pulmonary venous hypertension determines, the clinical presentation. Patients with severe obstruction may present, with hypoxia, cyanosis and dyspnoea caused by pulmonary oedema,, , 289, Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 2 : 290, , SECTION A The Chest and Cardiovascular System, , whilst patients with less severe obstruction may remain pink but, may present later with failure to thrive., The following three physiological states predominantly account for, patients with cyanosis., 4. Low Pulmonary Blood Flow: Reduction in pulmonary blood flow, is commonly caused by obstruction to outflow from the right ventricle, (RV), e.g. TOF or severe pulmonary stenosis (PS). The increased, resistance to RV outflow results in a redirection of systemic venous, return to the left heart (right to left shunt) via an interatrial communication (patent foramen ovale or ASD) or a VSD. Elevated, pulmonary vascular resistance (PVR) without anatomical obstruction, may also result in shunt redirection. As lung function is normal,, any pulmonary venous blood returns to the left atrium fully saturated, and mixes with the shunted systemic venous blood; however, because, pulmonary flow is so low, there is insufficient oxygenated blood in, the mix, resulting in cyanosis., 5. Parallel Circulations: This occurs in transposition of the great arteries, (TGA), where the aorta arises from the morphological right ventricle, and the pulmonary artery from the left ventricle. In this condition,, deoxygenated systemic venous return recirculates into the aorta and, the oxygenated pulmonary venous return recirculates to the pulmonary artery, a situation clearly incompatible with life. Patients, can only survive if there is sufficient mixing of the streams (shunt);, this can occur best at atrial level through a large interatrial communication, less well at ventricular level (via a VSD) and even less, well at great vessel level (via a PDA). Critical cyanosis may be managed, medically by maintaining patency of the PDA by prostaglandins,, but may require the creation of an artificial interatrial communication, using cardiac catheterisation until definitive treatment by surgically, switching the great vessels., 6. Intracardiac Mixing: Complete intracardiac mixing of blood may, occur at atrial level (common atrium), ventricular level (all univentricular hearts) or great artery level (common arterial trunk). Patients, are expected to be mildly cyanosed, depending on the relative amount, of deoxygenated blood in the mix, and breathless, according to the, amount of pulmonary blood flow., , Later Clinical Presentation, The majority of adult patients with CHD are survivors from childhood., This group may present with an interesting array of problems related, to residual lesions or deteriorations of their initial repair or palliation, (heart failure, valve regurgitation, conduit stenosis, baffle leaks). They, require life-long surveillance for anticipated problems arising from the, ‘unnatural history’ of their underlying disorder., New presentations of CHD continue beyond infancy into adulthood, usually because the underlying disorder has not yet produced, symptoms. Common lesions include left-right shunts, such as ASDs,, VSDs or partial anomalous pulmonary venous drainage, which only, begin to be symptomatic in older patients; milder forms of LV or aortic, obstruction such as coarctation of the aorta or valvular AS, which did not, compromise systemic perfusion, may progress and become symptomatic, in later childhood or adulthood; and milder forms of RV obstruction, such as PS. A very rare late presentation of CHD is congenitally corrected, TGA (atrioventricular (AV) and ventriculo-arterial discordance). Here,, the right atrium connects to the left ventricle, then the pulmonary trunk,, and the left atrium to the right ventricle, then the aorta. Whilst blood, flow is ‘normal’, the right ventricle is the systemic ventricle and may fail, late in life or even found to be undiagnosed until a post-mortem study., An important presentation for unrepaired CHD is that of pulmonary, arterial hypertension (PAH). PAH is a common complication of adult, congenital heart disease (ACHD), affecting up to 10% of patients. PAH, related to CHD is characterised by a rise in PVR with normal left atrial, , pressure. It is typically the result of pulmonary vascular disease caused by, chronically elevated pulmonary arterial pressures in patients with large, post-tricuspid defects such as VSDs, PDAs or aortopulmonary windows., Chronic pressure and volume load cause proliferative lesions to develop, in the small muscular pulmonary arteries, which result in elevated PVR., Clinical features include signs of elevated pulmonary artery (PA) pressure, and subpulmonary (usually RV) maladaptation (Fig. 13.1)., Clearly, life-limiting conditions such as parallel circulation, significant, shunts, severe intracardiac mixing or compromised systemic perfusion, would not normally be expected beyond childhood., SUMMARY BOX: Major Modes of Clinical Presentation of, Congenital Heart Disease, • Left-to-right shunt (e.g. ASDs, VSDs, PDA)., • Compromised systemic perfusion (e.g. critical aortic stenosis)., • Pulmonary venous congestion (e,g, obstructed TAPVD)., • Low pulmonary blood flow (e,g, tetralogy of Fallot)., • Parallel circulation (e,g, transposition of the great arteries)., • Intracardiac mixing (e,g, truncus arteriosus)., ASDs, Atrial septal defects; PDA, patent ductus arteriosus;, TAPVD, total anomalous pulmonary venous connection;, VSDs, ventricular septal defects., , MORPHOLOGICAL DESCRIPTION AND SEQUENTIAL, SEGMENTAL ANALYSIS, A significant diversity of morphological abnormalities may be responsible, for the physiological phenomena described above and although initial, management of an infant simply requires correct classification of the, initial physiological pattern, subsequent surgical correction and medical, management requires a precise anatomical diagnosis. The potential, intrinsic complexity of CHD necessitates a systematic scheme of, nomenclature that captures precisely the unique anatomy of each patient,, called sequential segmental analysis. Using this approach, the clinician, describes how the components of the heart and blood vessels are connected. This entails describing atrial situs (location of the atrial chambers, and whether they are of left or right morphology), atrioventricular, (AV) connections, ventriculo-arterial (VA) connections and other, associated lesions in turn. Any cross-sectional imaging technique may, be used for this purpose but transthoracic echocardiography is most, commonly used for routine inpatient and outpatient assessment. In, more complex lesions or when echocardiography provides an inadequate, assessment (e.g. poor acoustic windows), CMR represents a powerful, non-invasive technique giving morphological and haemodynamic, information that echocardiography alone cannot provide., , Sequential Segmental Analysis, Step 1—Atrial Situs, , Atrial situs is determined by an assessment of the morphology of, each atrial appendage. Correct identification of the atrium allows the, subsequent determination of the AV connection. The atrial appendages, are the most consistent feature of the atrial mass; indeed, the venous, attachments to each atrial chamber can form a variety of combinations., The right atrial appendage is a triangular shape, with a broad base and, prominent pectinate muscles that extend around the right AV valve, whilst, the left atrial appendage is a more elongated, tubular structure and has, less extensive pectinate muscles that are confined within the appendage., The most common lesions involve inversion of situs, or isomerism, of the left or right atrial appendages. The non-cardiac thoracic and, abdominal organs usually (but not always) demonstrate a similar ‘sidedness’ to that of the atrial chambers., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 3 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , A, , B, , C, , D, , 291, , Fig. 13.1 A 7-Year-Old Child With Pulmonary Arterial Hypertension and an Atrial Septal Defect., (A) Tricuspid regurgitation velocity 4 m/s, indicating an estimated right ventricular (RV) systolic pressure of, 64 mm Hg + right atrial pressure. (B) Dilated and hypertrophied RV. (C) Abnormal interventricular septum, curvature in late RV systole consistent with elevated RV systolic pressure. (D) Phase-contrast flow curve in, right pulmonary artery. Arrow indicates mid-systolic ‘notch’ caused by pathological wave reflection arising, in the abnormal pulmonary vasculature., , In the normal heart the morphological right atrium is located to, the right of the morphological left atrium (situs solitus). The right lung, is trilobed, with a shorter, early-branching bronchus and the left lung, is bilobed. In addition, the inferior vena cava (IVC) is to the right of, the abdominal aorta, with a right-sided liver and left-sided spleen., In situs inversus the mirror image of the normal anatomy is present., Isomerism of the left atrial appendages is usually associated with, bilateral bilobed lungs, polysplenia and IVC interruption. Isomerism, of the right atrial appendages is usually associated with bilateral triilobed, lungs, asplenia and a midline liver. In isomeric lesions there is often a, common AV junction (instead of two separate and offset left and right, junctions) with varying degrees of AV septal defect (AVSD). Gut malrotation is associated with both right and left-sided isomerism., , Step 2—Ventricular Morphology, Determination of ventricular morphology allows analysis of AV and, ventriculo-arterial connections. An AV connection is described as, ‘concordant’ when the atria are connected to the expected ventricle (i.e., left atrium with left ventricle and right atrium with right ventricle);, ‘discordant’ if the left atrium is connected to the right ventricle and, right atrium to the left ventricle; ‘ambiguous’ if there is isomerism of, the atrial appendages (e.g. two morphologically right atria connected, , to a left and right ventricle, respectively (one connection is concordant,, the other discordant)); and, finally, ‘univentricular’ if both atria predominately connect to a single ventricle. Irrespective of AV concordance,, the AV valve is always concordant with the ventricle—that is the tricuspid, valve connects to the morphological right ventricle and the mitral valve, connects to the morphological left ventricle., The most distinguishing feature of the tricuspid valve is the direct, attachments to the septum of cords from the septal leaflet. Unlike the, tricuspid valve, the mitral valve has no direct septal attachments. The, septal insertion of the tricuspid valve is more apical (apically ‘offset’), than that of the mitral valve and these features aid determination of, the ventricular morphology. The muscular structure of the ventricles, also differs, with the RV being more trabeculated than the LV, with a, muscular infundibulum and mid-ventricular ‘moderator band’. Although, they are different in normal subjects, the size, shape and degree of, trabeculation of the ventricles are not good indicators of ventricular, origin, as all are dependent on load effects., , Step 3—Ventriculo-Arterial Connection, Description of ventriculo-arterial connections represents the final, element of sequential segmental analysis. This entails describing how, each great vessel (aorta, pulmonary artery [PA], or common trunk) is, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 4 : 292, , SECTION A The Chest and Cardiovascular System, , connected to its respective ventricle. A ventriculo-arterial connection, may be concordant (RV-PA, LV-aorta), discordant (RV-aorta, LV-PA),, double outlet (e.g. RV-PA and aorta) or single outlet (e.g. LV and, RV to common arterial trunk). The aorta and pulmonary arteries, are defined by their typical branching patterns. Three-dimensional, balanced steady-state free-precession (b-SSFP) and contrast-enhanced, magnetic resonance angiography (MRA) techniques are particularly, useful in determining the arrangement of the great vessels and the, connections with their respective ventricles., , Flow: Using phase-contrast MRI, blood flow and its direction (mL/, beat) across valves and vascular structures can be quantified. In, valvar regurgitation, backward flow can be measured and expressed, as a regurgitant fraction (backward flow/forward flow). Combined, with cine imaging, flow data can be used to calculate and localise, intra-/extracardiac shunts., , Step 4—Identification of Other Abnormalities, , Imaging is fundamental to the diagnosis of CHD and is required at all, stages of patient care. An ideal non-invasive technique for imaging of, CHD should be able to accurately and reproducibly delineate all aspects, of the anatomy, including intracardiac abnormalities and abnormalities, of extracardiac vessels; evaluate physiological consequences of CHD, such as measurement of blood flow and pressure gradients across stenotic, valves or blood vessels; be cost-effective and portable; provide data, from fetal life to adulthood; not cause excessive discomfort and morbidity;, and not expose patients to harmful effects of ionising radiation. No, single technique has fulfilled these entire requirements and in the delivery, of a CHD service, the imaging techniques discussed below play an, important complementary role., , Other abnormalities to be considered include abnormal systemic and, pulmonary venous connections, intracardiac shunts, valvar abnormalities, and vascular abnormalities (PDA, right/left aortic arch, coarctation/, interruption or pulmonary arterial abnormalities)., In general, most congenital cardiac lesions are single abnormalities, that are easily described; however, almost any combination of abnormalities and connections can occur, and using the sequential segmental, analysis method, the description of all conceivable combinations, and diagnoses is possible. For more advanced reading, the reader, is referred to the textbook Paediatric Cardiology by Anderson and, colleagues (see Further Reading)., , NON-INVASIVE IMAGING TECHNIQUES, , Echocardiography, SUMMARY BOX: Summary of Sequential Segmental Analysis, 1. Describe the atrial arrangement., 2. Describe the type of atrioventricular connection., 3. Describe the ventriculo-arterial connection., 4. Describe the position of the heart (particularly if abnormal or unexpected)., 5. Describe associated abnormalities (e.g., venous abnormalities, septal defects,, valvar lesions, great vessel and coronary abnormalities)., 6. Describe acquired or iatrogenic abnormalities, , PHYSIOLOGICAL AND FUNCTIONAL ASSESSMENT, Whilst the correct morphological analysis is a critical first step, it must, be incorporated into a complete physiological assessment to understand, the clinical problem. It is helpful to briefly consider a few parameters, relating to normal cardiac function, which are commonly calculated, by techniques such as CMR., Stroke Volume: This is the volume of blood (mL) pumped (displaced), by a ventricle with each heartbeat. The displaced volume is calculated, by subtracting the volume of the ventricular cavity at end diastole, from the volume at end systole. In the normal heart the stroke, volume for each ventricle is the same and is also the same as the, forward flow in the associated great artery. It may not be the same, in the presence of a shunt or a regurgitant valve. Here, discrepancies, in interventricular volumes or great artery flows help locate and, quantify the severity of shunts and valve regurgitation., Cardiac Output: This is how much blood each ventricular chamber, pumps in 1 minute (L/min). It is calculated by multiplying the stroke, volume (or great artery flow (mL)) by the heart rate (stroke, (beat)/min). Cardiac output is increased by physiological stress (e.g.,, exercise that increases both heart rate and stroke volume) and, depressed in conditions that reduce either heart rate (bradyarrhythmias) or stroke volume (dilated cardiomyopathy, heart failure)., Ejection Fraction: A useful assessment of gross systolic cardiac function, is the percentage of blood ejected from the heart during each beat., This is calculated by dividing the stroke volume by the end-diastolic, volume. Ejection fraction may be decreased if the systolic performance, of the ventricle is impaired (cardiomyopathy)., , Echocardiography is the initial imaging technique used in the evaluation, of patients with suspected CHD and should always be performed before, other techniques are used. In most patients, echocardiography alone, provides sufficient information to complete the diagnostic evaluation, using a sequential segmental and functional analysis. In UK clinical, practice, paediatric cardiologists have traditionally performed echocardiography; however, more recently, neonatologists and radiologists have, begun to use echocardiography in patients with suspected CHD where, paediatric cardiology services are not immediately available. Cardiac, anaesthetists also increasingly perform perioperative assessment using, transoesophageal echocardiography. For a more comprehensive discussion, of echocardiography in CHD, the reader is referred to Lai et al (see, Further Reading)., , Magnetic Resonance Imaging, As previously alluded, CMR probably provides the most comprehensive, assessment available from a single non-invasive imaging technique but, its immobility, cost and limited availability constrain its general applicability. In our clinical practice it is used to define the morphology and, physiology of the most complex CHD cases as well as providing routine, surveillance for patients with repaired CHD such as TOF and TGA., Extracardiac anatomy, including the great arteries and systemic veins,, can be delineated with high spatial resolution. Vascular and valvular, flow can be assessed, shunts can be quantified and myocardial function, can be measured accurately with high reproducibility, regardless of, ventricular morphology. Finally, CMR provides high-resolution, isotropic,, three-dimensional data sets. This allows for reconstruction of data in, any imaging plane, facilitating visualisation of complex cardiac anomalies, without the use of ionising radiation., The majority of CMR images are acquired using cardiac (vectorcardiograph) gating during a single breath-hold to reduce the artefacts, associated with cardiac and respiratory motion. For a complex case,, CMR is performed over approximately 1 hour, although this time can, be considerably reduced if a focused question is being addressed or by, the incorporation of newer real-time sequences., Imaging sequences can be broadly divided into:, • ‘Black blood’ spin-echo images, where signal from blood is nulled, and thus not seen—for accurate anatomical imaging., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
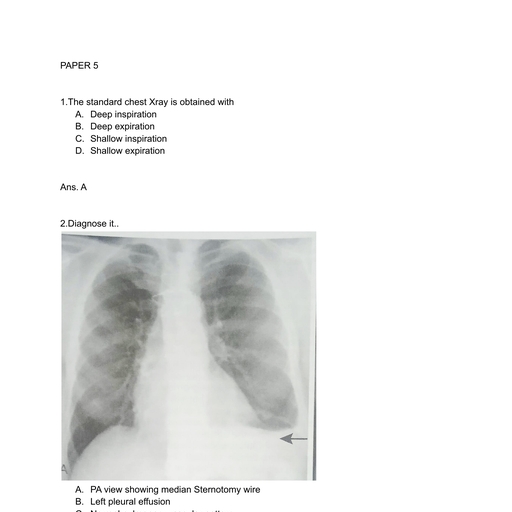
Page 5 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, •, , ‘White blood’ gradient-echo or SSFP images, where a positive signal, from blood is returned—for anatomical, cine imaging and quantification of ventricular volumes, mass and function., • Phase-contrast imaging, where velocity information is encoded for, quantification of vascular flow, including newer 4D (or 7D) phasecontrast imaging., • Contrast-enhanced MRA, where non-echocardiogram (ECG)-gated, 3D data are acquired after gadolinium contrast medium has been, administered for thoracic vasculature imaging., • Tissue characterisation imaging, where innate contrast between, normal myocardium and disease can be imaged: T1 mapping and, extracellular volume imaging, T2 oedema imaging, T2* iron deposition imaging, late gadolinium enhancement fibrosis and necrosis, imaging., All these sequences can be acquired in a single breath-hold, reducing, the overall time in the CMR machine and enabling the acquisition of, accurate data in the majority of patients. Importantly, ‘white blood’, cine images can be acquired in a continuous short-axis stack along the, heart, enabling accurate quantification of RV and LV function., Imaging should be performed in the presence of a cardiovascular, MRI clinician in conjunction with an MRI technician to ensure that, the appropriate clinical questions are answered. A comprehensive, treatment of cardiovascular MRI is provided in the textbook by Bogaert, and colleagues (see Further Reading)., , Computed Tomography, Cardiac CT is now well established for the assessment of the thoracic, vasculature and large and small airways. Recent advances in, multidetector CT (MDCT) with high-pitch spiral and volumetric scan, modes have resulted in significant advances in spatial and temporal, resolution and a decrease in radiation dose, often less than 1 mSv., Most studies are fully diagnostic without ECG gating. ECG-triggered, and ECG-gated acquisitions should therefore only be utilised when, cardiac motion may produce non-diagnostic images. Newer-generation, scanners permit rapid imaging with minimal motion artefact and thus, remove the need for gated scans and general anaesthesia. General, anaesthesia may still be needed to control breathing when detailed, coronary artery imaging is required., The route and contrast administration protocol are critical to successful imaging. The right upper limb in most cases provides a good, site of administration of contrast (avoiding streak artefact from contrast, in the innominate vein, which can obscure head and neck vessels)., Generally, a biphasic injection protocol using a power injector will be, appropriate, deploying a neat contrast bolus (1–3 mL/kg) followed by, saline chaser. In neonates and low-bodyweight children requiring small, absolute contrast doses, short contrast transit time increases the risk, of suboptimal opacification of essential structures. Using the full available, contrast dose, reducing the injection rate and mixing the contrast bolus, with saline increases the transit time. Empirically, dilution with saline, to 70%–80% contrast concentration gives good opacification., Visual bolus triggering from a low-resolution monitoring scan is our, favoured approach for timing of acquisition because it more reliably, ensures opacification of the appropriate cardiac structures. This does, incur a small, added radiation dose, which can be minimised by delaying, monitoring toward the end of the injection and reducing the frequency, of monitoring scans. A pre-scan timing bolus is often avoided because it, utilises part of the contrast bolus available and increases the radiation dose., We currently use MDCT for the following indications in patients, with CHD:, • Thoracic aorta disease, including vascular rings where airway information is critical. Aim for a narrow bolus via right arm injection to avoid, streak artefact from innominate vein over head and neck vessels., , 293, , •, , Pulmonary arterial disease. Aim for a prolonged contrast transit, time to ensure all sources of pulmonary blood supply are evaluated., The infradiaphragmatic area should also be imaged because collateral, vessels may arise here. If thromboembolic disease must be excluded,, a rapid undiluted bolus must reach the pulmonary arteries—this, can be extremely challenging in cavo-pulmonary connections., • Coronary artery abnormalities. ECG-triggered or ECG-gated protocols, may be necessary. Pharmacological heart rate reduction may be, required in cases of very high heart rate., • Pulmonary venous abnormalities. Aim for a prolonged contrast, transit time to ensure there has been ample time for delayed filling, of venous collaterals or slow flow segments. Care should be taken, to avoid very dense contrast that may cause streak artefact and obscure, anomalous entry points into the systemic venous system. The scan, should include the hepatic inferior vena cava in suspected infradiaphragmatic total anomalous pulmonary anomalous connections, or partial anomalous pulmonary venous drainage to the hepatic, inferior vena cava., • Patients with implants or devices that cannot be imaged by CMR., Imaging should take account of the material to be imaged. Higher, kVp, edge-enhancing reconstruction kernels and iterative reconstruction improve the diagnostic accuracy., The reader is referred to the expert consensus document on CT, imaging in patients with CHD of the Society for Cardiovascular, Computed Tomography (SCCT) (see Han et al., Further Reading)., , Conventional Radiology, Although CHD may be suspected on the basis of the chest x-ray (CXR),, the technique precludes the detailed morphological assessment necessary, for diagnosis and determination of specific underlying pathology., The diagnostic accuracy of the CXR in the assessment of infants, with asymptomatic murmurs is poor. Despite its poor performance as, a screening tool, CHD may be suspected on the basis of a CXR because, of higher specificity, but false-positive rates are significant., The CXR, however, is not dispensable and remains important in, the subsequent management of patients with CHD, particularly in three, situations:, 1. Postoperatively, for identification of the position of intravascular, catheters, chest drains and endotracheal tubes (Fig. 13.2A)., 2. Identification of postoperative complications: consolidation, collapse,, pleural effusion, pneumothorax, pneumomediastinum or pericardial, collections (see Fig. 13.2B)., 3. Perioperative, physiological assessment of the lungs and cardiomediastinal contour (see below)., , Diagnostic Features, The ubiquity of the CXR in clinical practice warrants discussion of the, diagnostic features that should prompt suspicion of CHD. It is suggested, that when reporting images, the reader avoid such terms as ‘boot-shaped’, or ‘snowman’ typically associated with specific lesions because they can, be misleading and often erroneous. More appropriate is a descriptive, consideration of the cardiomediastinal contour and lungs, attempting, to evaluate the predominant physiological profile discussed above. The, reader may find it helpful to read this section in conjunction with the, section on clinical presentation., , The Pulmonary Vasculature, Radiologically normal pulmonary vascularity is present in CHD if the, patient is not in heart failure, if no large shunt is present and if there, is no significant reduction in pulmonary blood flow: for example, mild, PS. The pulmonary vasculature may, however, look normal on the, conventional radiograph even in the presence of significant CHD., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 6 : 294, , SECTION A The Chest and Cardiovascular System, , A, , B, Fig. 13.2 Perioperative Chest X-Ray. (A) A 3-year-old patient following total cavo-pulmonary connection, surgery, postoperative chest x-ray demonstrating tube positions in intensive care. Note two chest and one, mediastinal drains, endotracheal tube and veno-venous collateral occluder device (right upper zone). (B) Third, postoperative day following extubation and removal of mediastinal drain. Note change in cardiomediastinal, contour caused by large pericardial clot, requiring evacuation., , B, , A, , Fig. 13.3 Physiological Assessment Using Chest X-Ray. (A) Pulmonary plethora in a patient with a ventricular, septal defect. Note the increased number and size of discrete vessels without haziness. (B) Pulmonary, oedema in a supine patient with cor triatriatum (membranous obstruction to left atrium outflow) resulting in, increased pulmonary venous pressure. Note cardiomegaly, perihilar alveolar haziness/consolidation and, peribronchial cuffing., , Increased pulmonary perfusion (pulmonary plethora) is recognised by, enlarged central and peripheral pulmonary arteries and veins in all zones, (Fig. 13.3A), as occurs in situations with increased pulmonary blood, flow: ASD, VSD and PDA with large left-to-right shunts (Table 13.1)., Decreased pulmonary perfusion (oligaemia) (Fig. 13.4) is caused by, a reduction in pulmonary blood flow and is typically a phenomenon, of cyanotic CHD. Dark lungs and sparse pulmonary vascular markings, , suggest the diagnosis. Image acquisition must be optimal because, overexposure will significantly confound correct interpretation. Pulmonary blood flow may be impaired by obstruction to normal flow, through the right heart: for example, tricuspid atresia, TOF and PS, (Table 13.2)., Pulmonary venous congestion and oedema (see Fig. 13.3B) in CHD, is caused by functional or anatomical obstruction to pulmonary venous, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 7 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , 295, , B, , A, , Fig. 13.4 Pulmonary Oligaemia. (A) Supine anterior-posterior (AP) chest x-ray (CXR) in an 8-week-old patient, with tetralogy of Fallot with severe pulmonary stenosis and cyanosis. Note black lungs with sparse, small-calibre, vessels. (B) Supine AP CXR in the same patient following construction of a right modified Blalock–Taussig, shunt on the next day. Note the increased size of the left cardiac contour caused by increased left ventricle, filling, increased pulmonary vascular markings, now plethoric, suggestive of high pulmonary blood flow arising, from the shunt. Indeed, the patient had compromised systemic perfusion caused by redistribution of cardiac, output to the lungs, necessitating clipping the shunt to reduce its calibre., , Increased Pulmonary, Perfusion (Plethora), , TABLE 13.2, , Level of Shunt, , Cardiac Lesion, , Level, , Cardiac Lesion, , Atria, , Ostium secundum ASDa, Ostium primum ASD (partial AVSD)*, Sinus venosus defect, Anomalous pulmonary venous drainage, (partiala; totalb), Complete AVSD, Partial AVSDa, VSDa, Double outlet ventricleb, Single ventricleb, PDAa, Aortopulmonary window, Common arterial trunkb, Coronary artery-RV fistula, Transposition of great arteriesb, Systemic to pulmonary artery shunts, (unrestrictive BT-shunt), Vein of Galen malformation, , Tricuspid valve, , Tricuspid atresia, Tricuspid stenosis, Ebstein anomaly, Pulmonary infundibular stenosis (severe), Pulmonary valvar stenosis (severe), Tetralogy of Fallot, Pulmonary artery atresia, Right or left pulmonary artery interruption, (differential lung oligaemia), Peripheral pulmonary artery stenosis, (regional oligaemia), Transposition of great arteries with, pulmonary valve stenosis, , TABLE 13.1, , Atrioventricular valves, Ventricle, , Great vessels, , Other, a, , Common cause of plethora without cyanosis., Common cause of plethora with cyanosis., ASD, Atrial septal defect; AVSD, atrioventricular septal defect;, BT, Blalock–Taussig; PDA, patent ductus arteriosus; RV, right, ventricle; VSD, ventricular septal defect., b, , return. In addition to oedema formation caused by increased transvascular pressure gradients, consideration should be given to other pathological processes such as increased vessel leakiness caused by acute lung, injuries, for example (Table 13.3). The usual adult pattern of basal, oedema, resulting in alveolar hypoxia and constriction of lower, , Oligaemia, , Right ventricular outflow, , Pulmonary artery, , Neonatal Pulmonary, , pulmonary vasculature and redirection to the apices does not apply to, the supine infant. As pulmonary venous pressure increases, there is, progressive accumulation of radiological signs, beginning with redistribution (in older children/adults), progressing to interstitial oedema, (perivascular haziness, peribronchial cuffing, Kerley B lines, subpleural, effusions) and, finally, migration of extravasated fluid centrally, resulting, in perihilar alveolar consolidation., Systemic to pulmonary collateral vessels. Abnormal systemic arterial, connections to the pulmonary vasculature may occur as an adaptive, mechanism to inadequate pulmonary blood flow. This usually occurs, in the setting of pulmonary atresia associated with VSD, in which the, RV and pulmonary arteries are not in continuity; instead, discrete, MAPCAs (major aortopulmonary collateral arteries) and non-discrete, networks of bronchial arteries are the source of pulmonary blood flow., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
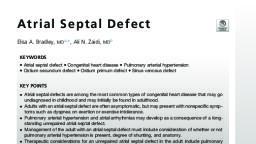
Page 8 : 296, , SECTION A The Chest and Cardiovascular System, , Pulmonary Oedema and, Venous Congestion, TABLE 13.3, Level, , Cardiac Lesion, , Pulmonary veins, , Obstructed TAPVD, Pulmonary vein stenosis, Cor triatriatum, Mitral valve stenosis/atresia, Left atrioventricular valve regurgitation, Hypoplastic left ventricle, LV endocardial fibroelastosis, Cardiomyopathy, LV ischaemia-aberrant left coronary artery, from pulmonary artery (ALCAPA), Aortic stenosis/atresia, Coarctation/interruption of the aorta, Asphyxia, Acute lung injury, Intravenous overhydration, , Left atrium, , Left ventricle, , Aorta, Non-cardiac pulmonary, oedema, , LV, Left ventricle; TAPVD, total anomalous pulmonary venous, connection., , It may also occur during staged management of the single ventricle., They may be recognisable by a nodular lung pattern in the central third, of the lung parenchyma, with many small, rounded, opacities representing, enlarged bronchial arteries seen end-on., Pulmonary arterial hypertension may complicate unrepaired CHD., Increased pulmonary blood flow caused by left-right shunting in, unrepaired ASD, VSD or PDA gradually causes changes in the pulmonary, vasculature, which, over time, leads to increased PVR and overt hypertension. The central pulmonary arteries enlarge and the peripheral pulmonary arteries become smaller than normal. In cases where pulmonary, pressure exceeds systemic pressure, shunt reversal occurs, resulting in, cyanosis—as occurs in Eisenmenger syndrome., , Heart Size, Shape and Position, Abnormalities of the position of the cardiac apex, aortic arch, liver and, stomach may be determined from examination of the CXR. The presence, of situs inversus and left aortic arch may be discerned; however, this, may or may not be associated with underlying CHD. Some assessment, of global and regional heart size is possible (see Fig. 13.3B) and should, be described; however, the limitations of CXR in this regard should be, considered. In a study comparing echocardiographical assessment of, cardiac enlargement in 95 consecutive paediatric outpatients, the sensitivity of the CXR to identify cardiomegaly was only 58.8% (95% confidence, index (CI): 32.9 to 81.6), specificity was 92.3% (95% CI: 84.0 to 97.1)., , SPECIFIC LESIONS, In the following discussion lesions have been classed as acyantoic and, cyanotic for convenience. It is important to understand, however, that, in various situations a lesion typically described in this way may present, in the opposite manner, perhaps caused by the presence or absence of, a particular morphological feature or the imposition of altered haemodynamics such as elevated PVR. For example, TOF with minimal outflow, tract obstruction may have no cyanosis or a VSD that is so large as to, facilitate complete intracardiac mixing may produce cyanosis. Furthermore, certain lesions do not fit easily into either category: for example,, Ebstein anomaly of the tricuspid valve when mild is acyanotic but in, its severe form is cyanotic. Similarly, congenitally corrected TGA, although, acyanotic, is better understood when discussed alongside its cyanotic, , relative, simple TGA. For further illustrations and images, the reader, is referred to the imaging atlas on CHD by Sridharan et al (see Further, Reading)., , ACYANOTIC LESIONS, Septal Defects, Atrial Septal Defects, ASDs are the most common congenital heart defect detected in adults., Irrespective of their type and location, isolated ASDs cause left-to-right, shunting at the atrial level. This leads to atrial dilation, predisposing, to tachyarrhythmias, and RV volume overload. The degree and direction, of atrial shunting can be modified by AV valve function and ventricular, compliance. The presence of an ASD is an independent risk factor for, thromboembolic stroke. This is caused by the ability of thromboemboli,, originating either in the right atrium or venous vasculature, to pass, through the ASD into the systemic circulation., ASDs are, anatomically and developmentally, a heterogeneous group, of lesions (Fig. 13.5A). The specific nature of the ASD influences the, natural history and management of this disease. Ostium secundum, defects make up 80% of ASDs and are located in the fossa ovalis (see, Fig. 13.5B). These defects are caused by failure of the septum secundum, to form closure of the ostium secundum. Other forms of ASD are more, properly termed interatrial communications because they do not occur, in the true morphological atrial septum. The ostium primum defect is, actually a component of a common AV junction, also known as an, AVSD. This defect usually occurs together with some degree of AV valve, abnormality. The sinus venosus defect is found at the junction of the, right atrium and either one of the caval veins (see Fig. 13.5C). This, type of ASD is less common and is always associated with partial, anomalous pulmonary venous drainage. The least common type of, ASD occurs in the coronary sinus and is termed an unroofed coronary, sinus. In this case, there is deficiency of the coronary sinus wall as it, passes behind the left atrium, allowing shunting from left to right through, the coronary sinus itself., The management of ASDs has changed in recent years, particularly, with the increasing use of transcatheter ASD closure devices. Previously,, surgical closure was only considered when a large left-to-right shunt, led to RV volume overload, atrial dilation and symptoms; however,, with the advent of transcatheter techniques, management has become, more aggressive. Transcatheter techniques are only viable in patients, with small-to-medium-sized ostium secundum defects that have adequate, margins with which to anchor the device. Deficiency of the anterior or, posteroinferior rim of the defect usually precludes transcatheter closure., Patients with large ostium secundum defects, or defects with deficiency, of the anterior or posteroinferior rim. or with sinus venosus lesions,, usually require operative repair. The clinical aim is to complete ASD, closure before the development of cardiac failure or atrial dilation and, timing of intervention depends on the haemodynamic status of the, patient; thus, evaluation of ASDs requires definition of type and location, of the defect, quantification of the net shunt (pulmonary flow: systemic, flow (Qp:Qs)), detection of any intra-atrial thrombus, assessment of RV, volume and systolic function and visualisation of the pulmonary venous, anatomy., Visualisation of most interatrial communications is possible by, transthoracic echocardiography, although sinus venosus or coronary, sinus defects are challenging without a high level of suspicion. In addition,, detection of pulmonary venous abnormalities is technically difficult, using the transthoracic approach. Transoesophageal echocardiography, is the main imaging technique used to assess ASDs (particularly at the, time of catheter and surgical closure); however, transoesophageal, echocardiography cannot be used to accurately quantify the shunt (Qp:Qs), , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 9 : 297, , CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , Superior sinus, venosus defect, , Primum ASD, , Secundum ASD, Inferior sinus venosus defect, , Coronary sinus defect, , A, , B, , 600, Aorta, Main PA, , Flow (mL/s), , 400, , 200, 100, , -200, , 0, , 300, , 600, Time (m/s), , C, , D, Fig. 13.5 Atrial Septal Defects. (A) Schematic drawing of atrial septal defect (ASD) positions. (B) Balanced, steady-state free-precession (b-SSFP) cardiac magnetic resonance (CMR) image. Four-Chamber view showing, a large secundum ASD with posterior extension. The absence of a posterior rim (arrow) precludes insertion, of an ASD closure device. Note the dilated right atrium (RA) and right ventricle (RV) and flattened interventricular, septum. (C) b-SSFP CMR image. Axial view showing a large superior sinus venosus defect with partial, anomalous pulmonary venous connection/drainage of the right upper and right middle pulmonary veins, straddling the deficient atrial septum (arrow). LA, Left atrium; RA, right atrium. (D) Plot of instantaneous flow, (measured by velocity-encoded phase-contrast magnetic resonance imaging) as a function of time showing, a left-to-right shunt through an ASD. Note increased pulmonary blood flow. PA, pulmonary artery., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved., , 900
Page 10 : 298, , SECTION A The Chest and Cardiovascular System, , and it can be difficult to delineate pulmonary venous anatomy. CMR, has, therefore, a significant role in the diagnosis and pre-interventional, assessment of ASDs., Three-dimensional whole-heart techniques, with isotropic resolution,, allow accurate multiplanar reformatting with no loss of resolution., These techniques allow 3D rendering of the atrial anatomy. Multislice, 2D gradient-echo techniques can be used to assess the dynamic 3D, anatomy of the defect, and phase-contrast through-plane flow techniques, can accurately size the cross-sectional dimensions of the defect. Multiple, or fenestrated defects may also be diagnosed., Haemodynamic assessment is also an important part of the evaluation, of ASDs. Invasive catheterisation has historically been used to quantify, left-to-right shunts. Quantification of left-to-right shunts using velocityencoded phase-contrast MRI compares well to invasive catheterisation, results (see Fig. 13.5D). It has the benefit of being non-invasive and, does not require exposure to ionising radiation. Ventricular overload, can also be accurately assessed using multislice b-SSFP short-axis, imaging and can give important information influencing the timing, of intervention., Key imaging goals, • Assess defect location, diameter and margin size—suitability for, device anchorage., • Quantify right heart volume and function—assess volume overload., • Quantify shunt (see Fig. 13.5D)., • Look for sinus venosus defect, which has an associated partially, anomalous pulmonary venous drainage., • Look for signs suggestive of elevated PVR—RV hypertrophy, systolic, flattening of the interventricular septum and notching of the pulmonary artery flow curve., , Atrioventricular Septal Defects, An atrioventricular septal defect (AVSD) is a lesion caused by a deficiency, of the tissues that normally interpose the atrial and ventricular chambers, (Fig. 13.6A and C). The involved tissues include the atrial primum, septum, the AV valves and the inlet portion of the ventricular septum., The feature shared by all AVSDs is a common AV junction guarded by, a common AV valve, which may have either one or two orifices (see, Fig. 13.6A)., , RAS, , The common AV junction can be discerned by the loss of the usual, ‘offset’ of the tricuspid and mitral valves in the normal heart. The valve,, even when it has two orifices, is no longer referred to as a mitral and, tricuspid valve; instead they are called left and right AV valves. The, common valve typically has five leaflets, referred to as the superior, bridging, right anterosuperior, right inferior/mural, inferior bridging, and left mural leaflets (see Fig. 13.6AB)., The relative deficiency of the septal structures and the number of, valve orifices give rise to the classification as complete (both ASD and, VSDs and single valve orifice), intermediate/incomplete (VSD with, two valve orifices) and partial (ASD with two valve orifices, also called, an ostium primum ASD). Another clinically useful description is the, relative size of the ventricular chambers, allowing for classification, as balanced (equal-sized ventricles) or unbalanced (disproportionate, ventricles). AVSD can be associated with other cardiac abnormalities,, including TOF, subaortic stenosis, atrial isomerism and ventricular, hypoplasia, which modify the presentation, prognosis and surgical, management., The diagnosis of AVSD is made in the neonatal period on the basis of, a transthoracic ECG. Other imaging techniques are usually not required., Surgical repair is carried out at approximately 3 to 4 months of age, and certainly before 6 months of age to prevent the development of, pulmonary vascular disease. The repair involves closing the septal defects, and creating competent left and right valves from the common AV valve, tissue. The association of AVSD with trisomy 21 is well known; repair, in this group is associated with lower mortality than non-trisomy 21., Additional imaging techniques including CMR may be useful in the, long-term management of patients with repaired AVSD, including, surveillance for important late complications such as AV valve regurgitation (see Fig. 13.6C)., Key imaging goals, • Assess ventricular proportion—unbalanced ventricle may not be, suitable for biventricular repair., • Assess valve structure., • Identify associated abnormalities—isomerism of the atrial appendages., • Quantify ventricular volume and function., • Quantify shunt., • Evaluate AV valve regurgitation., , SB, , LM, , A, , RI, , IB, , B, , C, , Fig. 13.6 Atrioventricular Septal Defects. (A) Schematic drawing of orthogonal views of a common atrioventricular valve: Short-axis view from below (left), Long-axis (top right), four-chamber (bottom right)., (B) Valve view showing a complete atrioventricular septal defect (AVSD) in a patient with right atrial isomerism, and double outlet right ventricle. Valve leaflets: IB, inferior bridging leaflet; LM, left mural leaflet; RAS, right, anterosuperior leaflet; RI, right inferior (mural) leaflet; SB, superior bridging leaflet. (C) Balanced steady-state, free-precession cardiac magnetic resonance image showing four-chamber view of a balanced complete, AVSD. There are large atrial and ventricular components. Note the VSD (arrow) and moderate left AV valve, regurgitation (arrowhead)., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 11 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, •, , Ventricular Septal Defects, The ventricular septum is a complex, almost helical 3D structure. VSDs, are the commonest form of CHD in childhood (Fig. 13.7). Physiologically,, the defect causes left-to-right shunting and the magnitude of the shunt, determines the signs and symptoms. The volume of the shunt depends, on the size of the defect and the relative resistances of the systemic and, pulmonary circulations; at birth the PVR is high, reducing the magnitude, of the shunt (it also remains high for longer in patients with left-to-right, shunts, explaining why infants may initially be asymptomatic). The, degree of shunting is usually estimated by measuring the velocity of, blood crossing the defect by ECG; if PVR is normal, higher-velocity, jets indicate that the expected pressure difference between chambers is, preserved and are termed ‘restrictive’ defects; low-velocity jets suggest, the LV and RV have similar pressures and that the defect is ‘unrestrictive’., The exact volume of the shunt cannot be determined accurately by, ECG, but can be qualitatively inferred by relative chamber dilatation., As described above for ASDs, shunt volume can be measured using, velocity-encoded phase-contrast CMR (see Fig. 13.5D)., The commonest location is the perimembranous region, accounting, for 80% of VSDs; many small perimembranous VSDs close spontaneously., The rest of the ventricular septum is muscular and has three components:, inlet, outlet (subarterial) and midmuscular regions (see Fig. 13.7A). The, appropriate management depends on the type and size of the defect., ECG is the mainstay of diagnosis but CMR can provide accurate 2D, and 3D images, which are particularly useful in complex defects. Multislice 2D gradient-echo techniques can be used to assess the dynamic 3D, anatomy of the defect; however, multislice techniques suffer from poor, through-plane resolution. Three-dimensional b-SSFP techniques with, isotropic resolution allow accurate multiplanar reformatting, permitting, 3D rendering of the ventricular anatomy. Image acquisition during the, diastolic period is useful in assessing the anatomy of a VSD and its, relationship to valvular structures (see Fig. 13.7B)., Key imaging goals, • Assess position and size of defect(s)., • If outlet VSD, describe commitment to a particular vessel: subaortic,, subpulmonary (see Fig. 13.7B)., , •, , •, •, •, , Quantify shunt (note LV stroke volume contributes to the PA forward, flow during systole)., Look for signs suggestive of elevated PVR—RV hypertrophy, systolic, flattening of the interventricular septum and notching of the pulmonary artery flow curve., Quantify ventricular volume., Assess aortic valve regurgitation and associated abnormalities., Post repair, assess integrity of VSD patch (see Fig. 13.7C)., , Abnormalities of the Great Vessels, Patent Ductus Arteriosus, , The arterial duct, in fetal life, connects the pulmonary artery to the, aortic arch, allowing blood ejected from the RV to bypass the highresistance pulmonary circulation and enter the descending aorta. The, ductal tissue constricts after birth in response to changes in the blood, gas composition. If the duct fails to close beyond the first few days of, life, it is termed a PDA. The PDA permits a left-to-right shunt from, the aorta into the pulmonary artery throughout the cardiac cycle. This, leads to increased pulmonary blood flow and dilation of the left heart., The length and diameter of the PDA and the relative resistances of the, pulmonary and systemic circulations determine the volume of the shunt,, which, in turn, determines the signs and symptoms of the lesion., A common neonatal problem is the failure of the ductus arteriosus, to close in the premature infant. In this situation, a PDA can confound, the management of the lung disease associated with prematurity and, can prolong ventilation. It can be comprehensively assessed using an, ECG in infancy but in older patients the duct may not be easily demonstrated. CMR may be required to visualise and quantify the shunt, in the same way as described for ASD and VSD., Key imaging goals, • Assess position and size of defect(s)., • Quantify shunt., • Assess for signs of elevated PVR—RV hypertrophy, systolic flattening, of the interventricular septum and notching of the pulmonary artery, flow curve., • Quantify volume overload., • Identify any associated intracardiac abnormalities., , Perimembranous VSD Doubly committed, subarterial VSD, Muscular, outlet VSD, , A, , Muscular, inlet VSD, , Apical muscular VSD, , B, , 299, , C, , Fig. 13.7 Ventricular Septal Defects. (A) Schematic drawing of ventricular septal defect (VSD) positions, viewed from the right ventricular aspect. (B) Balanced steady-state free-precession image of a VSD (arrow), with over-riding aorta in a patient with tetralogy of Fallot. (C) Coronal oblique view following correction with, VSD patch (arrowhead)., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 12 : 300, , SECTION A The Chest and Cardiovascular System, , Coarctation of the Aorta, , Interrupted Aortic Arch, , Coarctation of the aorta is a luminal narrowing of a short section of, the aorta (Fig. 13.8A–D). It occurs most commonly at the site of insertion, of the ductus arteriosus and is thought to develop because of the presence, of excessively integrated ductal tissue around the aortic isthmus, which, contracts along with the ductus arteriosus at the time of birth. In severe, coarctation, systemic perfusion will be compromised with ductal closure, in infancy caused by increased luminal narrowing and the loss of the, anatomical bypass provided by the duct itself. In less severe coarctation,, the body maintains perfusion by renal mechanisms, resulting in systemic, hypertension manifested proximal to the coarctation. Collateral arterial, vessels develop over time to maintain lower body perfusion as the patient, grows (see Fig. 13.8A and C). Patients may present with unexplained, hypertension as a teenager or adult and are at increased risk of the, attendant micro- and macrovascular complications., Treatment in infancy is usually by surgical excision of the narrowing, but in older subjects, balloon angioplasty may be undertaken. Patients, remain at increased risk of hypertension even if repaired in infancy., An ECG is used in the initial diagnosis of infants, children and, adults. Typical ECG features include increased systolic and diastolic, velocities across the stenosis (see Fig. 13.8D). CMR or CT may be required, in the postoperative phase to establish if there is re-coarctation (up to, 35% of patients in some series), aneurysmal dilatation or LV hypertrophy, secondary to hypertension. CMR is preferred to CT if there are no, contraindications., Imaging is crucial to establish the location and degree of stenosis,, length of coarctation segment (see Fig. 13.8B), associated aortic arch, involvement (such as tubular hypoplasia), the collateral pathways (internal, mammary and posterior mediastinal arteries), presence and relationship, to an aberrant subclavian artery, post-stenotic dilatation and LV, hypertrophy., Three-dimensional contrast-enhanced MRA can show the severity, and extent of involvement (see Fig. 13.8C). An assessment of collateral, flow by measuring flows in the proximal and descending aorta can be, performed. Reassessment of collateral flow following treatment can, also be used to assess the success of the treatment. In patients with, metal stents, high flip angle gradient-echo sequences can be used to, overcome metal artefact and assess luminal narrowing., CMR can also be used to assess secondary pathology in patients, with coarctation: for example, aortic root for dilatation associated with, a bicuspid aortic valve (frequency in coarctation of 15%), aortic valve, incompetence and stenosis and ventricular function and LV mass (an, indirect indicator of increased LV afterload)., Late after repair, imaging is used to assess for re-coarctation (especially, in hypertensive patients), pseudoaneurysm and dissection. Thoracic, aorta morphology is highly variable and represents the combination, of repair-type residual hypoplasia, stenosis and dilatation (Fig. 13.9)., Key imaging goals, • Describe location and degree of stenosis (MR flow mapping) and, length of coarctation segment., • Look for aortic root involvement and post-stenotic dilatation., • Assess aortic valve—often bicuspid., • Delineate collateral vessels., • Describe head and neck anatomy., • Assess ventricular function, volume and LV mass., • After repair also look for re-coarctation or pseudoaneurysm., • Assess calibre of stented vessels (high flip angle gradient-echo, or CT)., • Echocardiography—quantify Doppler-derived gradient across stenosis, and identification of ‘diastolic tail’ on continuous-pulsed-wave, Doppler flow profile (see Fig. 13.8D)., , Interrupted aortic arch results from a structural discontinuity between, the ascending and descending aorta. The site of interruption relative to, the brachiocephalic arteries forms the basis of classification. There is, a high incidence of DiGeorge syndrome, which is also associated with, variable thymic hypoplasia, the presence of which can be examined., Physiologically, systemic blood flow is provided distal to the interruption, by deoxygenated blood via a patent arterial duct. The lower body will be, cyanosed and circulation may be compromised following duct closure., The site and length of interruption and any associated anomalies can, be demonstrated well by CMR. Following repair, assessment is similar, to that of coarctation. It is important to interrogate the repair site for, residual narrowing, assess for the presence of LV outflow tract obstruction, due to posterior deviation of the outlet septum and look for residual, intracardiac shunts. Three-dimensional MRA and 3D whole-heart, imaging are particularly useful. Cine imaging will identify regions of flow, acceleration., Key imaging goals, • Describe the site of interruption and relationship of head and neck, vessels:, • Type A—interruption distal to the left subclavian artery (29%, of cases)., • Type B—interruption between the left common carotid and the, left subclavian (70% of cases)., • Type C—interruption between the innominate artery and the, left common carotid (1% of cases)., • Evaluate additional arch hypoplasia., • Measure aortic cross-sectional area proximal and distal to the, interruption., • Measure the distance of the interruption gap., • Identify associated anomalies—VSD, LVOT obstruction, TGA,, common arterial trunk., • Look for thymus—absence supports a diagnosis of DiGeorge, syndrome, , Abnormalities of the Aortic Arch and Vascular Rings, The aortic arch connects the ascending aorta to the descending aorta., Abnormalities of this vascular section include disorders of sidedness., Arch sidedness refers to the side of the trachea that the aortic arch passes, as it crosses a mainstem bronchus: namely, left, right and double. In, certain circumstances, the morphological pattern of the aortic arch and, related structures (its branches or the ductus/ligamentum arteriosus) may, produce a vascular ring, which can compress the trachea or oesophagus,, producing symptoms of stridor or dysphagia. This usually involves the, retro-oesophageal course of either the descending aorta or an aberrant, subclavian artery combined with a ligamentum arteriosus on the opposite, side of the arch, although non-ring structures such as anomalous origin of, the left pulmonary artery from the right pulmonary artery or ‘pulmonary, artery sling’ may also cause vascular compression., Cross-sectional imaging (CMR or CT) can be regarded as the gold, standard for the assessment of the aortic arch. For CMR, imaging begins, with a simple transverse stack from the level of the larynx to the diaphragm. This information is augmented by 3D MRA. Using this, information, patent vascular structures compressing the trachea/, oesophagus can easily be identified. It is important to remember that, some important components of a vascular ring may not be patent and, thus remain invisible on imaging—for example, the ligamentum, arteriosus; however, clues to these structures often remain and include, dimples opposite the side of the aortic arch, a diverticulum opposite, the side of the arch or if the proximal descending aorta descends on, the opposite side of the arch., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 13 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , A, , B, , C, , D, , 301, , Fig. 13.8 Severe Coarctation of the Aorta. (A) Posteroanterior chest x-ray showing characteristic bilateral, rib-notching (arrow) secondary to the development of collateral circulation. (B) Black blood, spin-echo oblique, sagittal image through the aorta showing a tight discrete coarctation (arrow). (C) Volume-rendered 3D, reconstruction of magnetic resonance angiography showing a tight coarctation (arrowhead), and multiple, enlarged collateral vessels. (D) Echocardiographic continuous-wave Doppler profile of the coarctation region,, demonstrating increased velocity across the stenosis, 4.18 m/s (blue cross), corresponding to a pressure, gradient of 70 mm Hg from the simplified Bernoulli equation. There is also markedly increased diastolic, velocity, characteristic in coarctation, termed ‘diastolic tail’ (red star)., , •, •, •, •, •, , Key imaging goals, Describe side of aortic arch., Delineate location and course of branches., Identify presence of associated PDA, or dimple suggestive of ligamentum arteriosus., Assess presence and level of compression of oesophageal/tracheal, compression., Identify associated abnormalities., , Valvular Heart Disease, Aortic Valve Disease, , Congenital aortic valve disease is predominated by stenosis, which may, occur at subvalvular, valvular or supravalvular levels. The haemodynamic, consequence of AS is pressure loading of the LV and the development of, secondary concentric hypertrophy. Aortic regurgitation (AR) is usually, a manifestation of treated AS (e.g. balloon angioplasty) or secondary to, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 14 : 302, , SECTION A The Chest and Cardiovascular System, , Fig. 13.9 Collage of Volume-Rendered Aortas from Patients with Repaired Coarctation of the Aorta., Note the highly variable morphology of the root, aortic arch and isthmus. Clinically and haemodynamically, relevant features include hypoplasia of the arch and re-coarctation. Patients are likely to have non-compliant, vessels, which predispose to hypertension., , pathological dilatation of the aortic root, which can occur in connective, tissue disease (e.g., Marfan syndrome, Fig. 13.10). The haemodynamic, consequence is volume loading of the LV and eccentric hypertrophy, (dilatation)., Doppler ECG assessment of transvalvular pressure gradient is the, commonest technique to assess severity of AS; however, transvalvular, pressure gradients are flow dependent and measurement of valve area, represents, from a theoretical point of view, the ideal way to quantify, AS. Inaccuracies in both gradients and valve area, however, require, consideration of a combination of flow rate, pressure gradient and, ventricular function, as well as functional status that may require, multimodality contributions. AS with a valve area less than 1.0 cm2 is, considered severe; however, in patients with either unusually small or, large body surface area, indexed areas, with a cut-off value of 0.6 cm2/m2,, is helpful. The presence of valvular stenosis can be identified by loss of, signal on CMR cine images. Velocity mapping can be used to establish, an accurate peak velocity across the stenosis, and planimetry can assess, the aortic valve area., An ECG is also used to routinely assess AR, in particular using, colour Doppler (to determine extension and width of regurgitant jet), and continuous-wave Doppler (to assess the rate of decline of aortic, regurgitant flow and holodiastolic flow reversal in the descending aorta);, however, these are semiquantitative measures. CMR permits precise, assessment of the regurgitant volume and assessment of the volume, and function of the eccentrically hypertrophied LV. It also allows assessment of the effective regurgitant orifice area., Subvalvular AS is the least common form of AS. It may be an isolated, lesion, or associated with hypertrophic cardiomyopathy or, occasionally,, following repair of AVSD. Valvular AS covers a broad spectrum of, anomalies, including critical AS presenting with compromised systemic, perfusion in infancy sometimes associated with the hypoplastic left-heart, syndrome, through to mild AS caused by a bicuspid aortic valve., Supravalvular AS is a rare lesion that is typically associated with, underlying Williams (Williams–Beuren) syndrome, a genetic disorder, of the connective tissue protein elastin. Elastin is responsible for the, normal distensibility of the aorta during systole and its subsequent, recoil during diastole. In Williams–Beuren syndrome, the reduced net, deposition of arterial wall elastin leads to increased proliferation of, , Fig. 13.10 Dilated Sinuses of Valsalva in a Patient With Marfan, Syndrome and Aortic Regurgitation., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 15 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, arterial wall smooth muscle cells and multilayer thickening of the medial, of large arteries, resulting in the development of obstructive hyperplastic, intimal lesions. A characteristic hourglass narrowing of the aorta develops, at the sinotubular junction but in approximately 30% of cases there is, a diffuse, tubular narrowing of the ascending aorta, often extending to, the arch and the origin of the brachiocephalic vessels., Key imaging goals, • Assess level and severity of stenosis, subvalvular, valvular,, supravalvular—MR flow mapping., • Assess valve leaflet structure (bicuspid valve)., • Quantify aortic regurgitation., • Evaluate aortic root dilatation/hypoplasia., • Quantify LV volume and systolic function., • Measure effective orifice area., • Identify other arterial stenosis—head and neck vessels and renal, arteries., • Echocardiography—quantify Doppler-derived gradient across stenosis, or width and extent of regurgitant jet in AR., , Pulmonary Valve Disease, Obstructive lesions dominate congenital pulmonary valve disease, similar, to the aortic valve, whereas significant pulmonary regurgitation (PR), is most often iatrogenic following surgical or catheter-based interventions, for obstructive lesions. Trivial PR is commonly discerned on an ECG, and can be considered physiological. Important congenital PR can occur, in the absent pulmonary valve syndrome., According to the site, PS is classified as valvular, subvalvular (infundibular) or supravalvular. It can occur as isolated finding or in constellation with other lesions such as VSDs or more complex lesions (TGA,, TOF), which may significantly alter the clinical presentation., PS and PR have physiological consequences analogous to aortic, valve stenosis and regurgitation. In the former, RV pressure rises to, overcome the obstruction and maintain stroke volume. Compensatory, mechanisms include RV hypertrophy. In PR, volume loading of the RV, results in progressive dilatation and dysfunction, which is associated, with adverse clinical outcomes., In pulmonary valve stenosis, the pressure gradient across the valve is, used to assess severity of the lesion more so than in left-sided valve conditions due in part to the difficulty of obtaining an accurate assessment, of pulmonary valve area. The systolic pressure gradient is derived from, the transpulmonary velocity flow curve using the simplified Bernoulli, equation (pressure gradient = 4 × velocity2). Mild stenosis is defined, by a peak velocity under 3 m/s on continuous-wave Doppler, which, corresponds to a peak gradient under 36 mm Hg; moderate stenosis, is defined by a peak velocity from 3 to 4 m/s, corresponding to a peak, gradient between 36 and 64 mm Hg; severe stenosis is characterised by, a peak velocity above 4 m/s, corresponding to a peak gradient above, 64 mm Hg. CMR assessment of PS can be performed in a similar fashion, as outlined for AS, above., CMR is the gold standard for the assessment of PR. As described, for AR, quantification of the regurgitant volume and its effect on the, RV can be precisely determined. RV volume and function cannot be, accurately assessed by 2D ECG but CMR measurements have been, shown to be associated with adverse outcomes and can aid decision, making for timing of interventions., Key imaging goals, • Assess level and severity of stenosis, subvalvular, valvular,, supravalvular—MR flow mapping., • Assess valve leaflet structure., • Quantify PR., • Evaluate main pulmonary artery dilatation/hypoplasia., • Quantify RV volume and systolic function., , •, •, , 303, , Measure effective orifice area., Echocardiography—quantify Doppler-derived gradient across stenosis., , Ebstein Anomaly of the Tricuspid Valve, Ebstein anomaly is a congenital abnormality of the tricuspid valve and, right ventricle with the following components: (1) adherence of the, tricuspid leaflets to the underlying myocardium (failure of delamination);, (2) anterior and apical rotational displacement of the functional annulus;, (3) dilation of the ‘atrialised’ portion of the right ventricle with variable, degrees of hypertrophy and thinning of the wall; (4) redundancy, fenestrations and tethering of the anterior leaflet; (5) dilation of the right AV, junction (the true tricuspid annulus); and (6) variable ventricular, myocardial dysfunction., The degree of displacement determines the clinical presentation. In, severe cases there is gross right atrial enlargement and raised right atrial, pressure. The anomaly is usually associated with an ASD and, therefore,, right-to-left shunting at the atrial level and subsequent cyanosis may, occur. Ebstein anomaly results in gross enlargement of the cardiac, contour with a prominent curved right atrial border on the plain chest, radiograph. Treatment is problematical, although expert surgical repair, of the tricuspid valve is possible in some centres. Imaging should assess, the valve morphology, quantify ventricular function and volume and, quantify right atrial enlargement., Key imaging goals, • Describe apical displacement of the septal leaflet of the tricuspid, valve., • Assess mobility of anterosuperior and inferior tricuspid valve, leaflets., • Note eccentric coaptation., • Quantify tricuspid regurgitation., • Quantify right atrium dilatation and size of atrialised RV., • Assess RV and LV volume, function and mass., • Quantify right-to-left shunt., • Exclude right ventricular outflow tract (RVOT) obstruction., , Coronary Artery Abnormalities, Anomalous Coronary Arteries, , Coronary artery abnormalities are rare. They involve anomalous proximal, and epicardial courses of the left coronary artery (LCA) and right, coronary artery (RCA) (Fig. 13.11) or, rarely, anomalous origin of the, LCA from the pulmonary artery (ALCAPA), Fig. 13.12. Anomalous, course is increasingly important when interventions are carried out in, close proximity to a coronary artery—for example, percutaneous, pulmonary valve implantation into the pulmonary trunk and compression of the LCA. Similarly, the course of the coronary arteries are, important during surgical repair of TOF; a transannular patch repair, may not be possible if the LCA arises from the RCA and passes anterior, to the RVOT tract., ALCAPA results in the LCA territory being supplied with low-pressure, deoxygenated blood; blood must therefore be supplied by collateralisation, from RCA. Patients experience myocardial ischaemia and usually present, approximately 4 to 5 months of age when PVR drops and LCA blood, flow is reduced. Patients with sufficient collateralisation may survive, to adulthood. Treatment usually involves surgical reimplantation of the, coronary artery using a button transfer technique or coronary artery, bypass grafting., From an anatomical point of view, coronary anomalies are classified, according to the coronary artery involved, the origin of the anomalous, coronary artery and the anatomical course of the proximal segment (see, Fig. 13.11). From a clinical point of view, the anomalies are divided into, ‘benign’ and ‘malignant’ lesions. The latter, especially those of ALCAPA, and in cases where the LCA arises from the RCA and passes between, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 16 : 304, , SECTION A The Chest and Cardiovascular System, , A, , B, , C, , D, , E, , F, , Fig. 13.11 Coronary Artery Anomalies. Schematic diagram of the coronary arteries viewed in the axial, oblique plane on CMR. (A) Anomalous LCX from RCA. (B) Anomalous RCA from left main stem (LMS), with, interarterial course between pulmonary artery and aorta. (C) Anomalous RCA from LMS passing posteriorly, between the aorta and atria. (D) Anomalous left coronary artery arising from RCA with interarterial course, between the pulmonary trunk and aorta. (E) Anomalous left coronary artery arising from RCA passing anterior, to pulmonary trunk. (F) Anomalous left coronary artery arising from RCA passing posteriorly between aorta, and atria. Ao, Aorta; LA, left atrium; LAD, left anterior descending artery; LCX, left circumflex artery; LV, left, ventricle; RA, right atrium; RCA, right coronary artery; RVOT, right ventricular outflow tract., , the aortic root and RVOT tract or pulmonary artery, have an increased, risk for developing myocardial ischaemia and sudden cardiac death., Even with multiple projections, the precise location of the proximal, course of the vessel in a patient with an abnormal origin of a coronary, artery can be difficult to depict with conventional angiography and, echocardiography; however, CMR and CT angiography provide reliable, visualisation of the root of the arteries and the coronary artery tree., Key imaging goals, • Delineate coronary artery anatomy—consider CT may be better,, Fig. 13.12A and B., • Look for myocardial perfusion defects—consider adenosine stress., • Identify areas of regional wall motion defects., • Assess ventricular function, volume and LV mass., • Identify mitral regurgitation—secondary to ischaemia., • Perform late gadolinium enhancement—to determine infarct size, if present, Fig. 13.12D., , CYANOTIC CONGENITAL HEART DISEASE, Tetralogy of Fallot, TOF is the most common cyanotic congenital heart defect, with an, incidence of approximately 420 per million live births. It is caused by, , malalignment of the muscular outlet septum, which leads to RVOT, obstruction, a subaortic VSD with aortic override and RV hypertrophy, (Fig. 13.13A–C). This produces the physiological pattern of low pulmonary blood flow and right-to-left shunt as described above. Current, management consists of early single-stage reconstructive surgery, with, closure of the VSD, and relief of the RVOT obstruction, usually by the, placement of a transannular patch (across the pulmonary valve annulus), to enlarge the RVOT. Staged reconstruction is still required if there is, severe cyanosis caused by a very narrow RVOT or significant hypoplasia, of the central pulmonary arteries. In such cases, a systemic-to-pulmonary, anastomosis called a modified Blalock–Taussig (BT) shunt is placed, (usually) between the innominate artery and the right pulmonary artery, (see Fig. 13.13D). This shunt is then taken down during subsequent, definitive repair., A transthoracic ECG is the imaging technique of choice for the, initial diagnosis and assessment of paediatric patients; however, CMR, imaging does have a role in untreated or shunt-palliated patients in, delineating pulmonary artery anatomy or excluding significant pulmonary, artery distortion. While early surgical mortality from complete repair, of TOF is very low in the modern surgical era, residual anatomical and, haemodynamic abnormalities are almost universal. These include right, ventricle dilatation from PR, RVOT aneurysm, RVOT obstruction,, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 17 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , A, , B, , C, , D, , 305, , Fig. 13.12 Anomalous Left Coronary Artery from Pulmonary Artery. (A) Computed tomography image, showing left coronary artery (LCA) origin from pulmonary artery (PA). (B) Volume-rendered image (arrow to, anomalous LCA from the pulmonary artery (ALCAPA). LPA, left pulmonary arteries; RV, right ventricle., (C and D) Short-axis balanced steady-state free-precession cardiac magnetic resonance image and corresponding, late gadolinium enhancement image from the same patient showing anteroseptal and papillary muscle, enhancement., , pulmonary artery stenosis, residual atrial or VSD, tricuspid valve, regurgitation and aortic root dilatation., CMR has emerged as the gold standard for the assessment of the, right ventricle in patients with repaired TOF. Two-dimensional b-SSFP, sequences can be used to define RVOT anatomy and quantitatively, assess RVOT dilatation or stenosis. Velocity-encoded phase-contrast, MR can accurately quantify the degree of PR and can be used to measure, peak velocities at the level of RVOT obstruction, as well as differential, regurgitation in the branch pulmonary arteries. MR assessment of RV, function/volumes with multislice short-axis b-SSFP imaging is particularly important when determining the timing and evaluating the impact, of invasive therapeutic strategies., Key imaging goals, • Describe the RVOT and pulmonary trunk anatomy., • Identify RVOT aneurysm., • Identify RVOT obstruction., • Quantify PR., • Assess branch PA anatomy and measure flow split., • Assess biventricular volume and function., • Exclude residual shunt (Qp:Qs)., • Measure aortic root for dilatation., • Delineate coronary artery anatomy (important for surgical or, percutaneous pulmonary valve replacement)., , Transposition of the Great Arteries, TGA is the second-commonest cyanotic CHD diagnosed in the first, year of life, with an incidence of 315 per million live births. In this, condition, the aorta arises from the right ventricle, and the pulmonary, artery from the right ventricle (ventriculo-arterial discordance) (Fig., 13.14A). This produces the physiological pattern of parallel circulations, described above, which is incompatible with life. Treatment for TGA, patients was revolutionised with the introduction of the Senning, procedure, in which an intra-atrial baffle was used to divert blood from, the right atrium to the left ventricle, and the left atrium to the right, ventricle. A variation to the Senning procedure, the Mustard procedure, uses a pericardial patch or prosthetic material to construct the intra-atrial, baffle; however, although both these procedures produce a physiologically, normal circulation, the patient is still left with a systemic RV. Patients, surviving with these repairs may have unique complications, including, pulmonary venous pathway or baffle obstruction, baffle leaks and failure, of the systemic RV. Currently, the arterial switch operation has become, the procedure of choice. In this operation, the great vessels are transected, above the valve sinuses and sutured to their appropriate ventricle; the, coronary arteries arising below this transection level must also be, transferred separately (see Fig. 13.14B). In cases of TGA associated with, a VSD and sub-PS, the Rastelli procedure (where blood from the LV is, channelled through the VSD to the aorta) is preferred., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 18 : 306, , SECTION A The Chest and Cardiovascular System, , A, , B, , C, , D, Fig. 13.13 Tetralogy of Fallot. (A) and (B) Right ventricular outflow tract, morphological specimen and, corresponding black-blood spin-echo image in coronal view. The deviated outlet septum (asterisk), aortic root, (arrowhead) and hypertrophied septoparietal trabeculations (arrow) are shown. (C) Balanced steady-state, free-precession image of unrepaired tetralogy of Fallot. Inflow/outflow view of the left ventricle shows a, ventricular septal defect with overriding aorta. Note the severe hypertrophy of the right ventricle. Ao, Aorta;, LV, left ventricle; RV, right ventricle. (D) Black-blood, spin-echo image of right modified Blalock–Taussig shunt;, 3.5 mm gortex tube from innominate artery to right pulmonary artery (arrow)., , •, , Key imaging goals, Arterial switch repair:, • Identify any RVOT or LVOT obstruction., • Assess branch pulmonary arteries, which may be narrowed as, they straddle the aorta (see Fig. 13.14C and D) (measure differential branch flow)., • Identify aortic root dilatation., , •, , • Assess coronary arteries for kinking, ostial stenosis., Mustard/Senning:, • Assess patency of baffle and pulmonary venous pathway., • Assess atrial baffles for leak (presence of shunt)., • Quantify systemic RV volume and function., • Perform late gadolinium enhancement for ventricular fibrosis/, scar., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 19 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , A, , B, , C, , D, Fig. 13.14 Transposition of the Great Arteries. (A) Balanced steady-state free-precession (b-SSFP) cardiac, magnetic resonance (CMR) image showing an oblique sagittal outlet view of the aorta arising from the right, ventricle (RV) and pulmonary artery arising posteriorly from the left ventricle (LV). (B) Schematic drawing of, the arterial switch repair of transposition of the great arteries, showing the Le Compte manoeuvre with the, translocation of the aorta and pulmonary artery. Note sites of coronary artery ‘button’ removal and subsequent, re-implantation into the neo-aortic root. (C) b-SSFP CMR image showing the pulmonary arteries straddling, the aorta following the arterial switch procedure with Le Compte manoeuvre. (D) Volume-rendered 3D, reconstruction of a contrast-enhanced magnetic resonance angiography showing bilateral proximal branch, pulmonary artery narrowing., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved., , 307
Page 20 : 308, , SECTION A The Chest and Cardiovascular System, , Congenitally Correct Transposition of the Great Arteries, , Pulmonary Atresia, , Congenitally corrected transposition of the great arteries (CCTGA) is, a rare disorder characterised by both AV discordance and ventriculoarterial discordance (right atrium to left ventricle to pulmonary artery, to lung (Fig. 13.15A) and left atrium to right ventricle to aorta). Therefore,, although the heart is anatomically abnormal, it is physiologically normal, in terms of the pulmonary and systemic circuits. This lesion does not, usually cause cyanosis; however, many of the problems are similar to, those experienced by patients with TGA, particularly those treated by, an atrial switch operation, and thus a systemic RV. CCTGA may be, asymptomatic and in some patients is an incidental finding; however,, the majority of patients with CCTGA have associated cardiac lesions, (see Fig. 13.15B), the most common being VSD. PS is present in, approximately 50% of cases and tricuspid valve abnormalities (e.g., Ebstein abnormality) are found in 20% of cases., Even without associated abnormalities, most patients with CCTGA, eventually develop systemic ventricular failure. The main role of imaging, is in evaluation of associated lesions, quantification of ventricular, function and assessment of postoperative complications., Key imaging goals, • Describe atrioventricular and ventriculo-arterial connections., • Identify associated VSD and tricuspid valve abnormalities., • Identify outflow tract obstruction., • Perform late gadolinium enhancement to assess for systemic RV, fibrosis or scarring., , Pulmonary atresia is the lack of luminal continuity and absence of, blood flow from the RV to the pulmonary artery. Pulmonary atresia, can be separated into two groups depending on the presence of a VSD., As the diagnosis and subsequent management of these two groups is, different, it is useful to consider them separately., Pulmonary atresia with a ventricular septal defect. This is the more, common variant and is considered by some to be a severe form of TOF,, with a subaortic VSD and overriding aorta. Pulmonary blood flow is supplied, via MAPCAs. Surgical repair aims to establish RVOT to the pulmonary, artery continuity with a homograft (RV-PA conduit), repair the VSD and, bring the aortopulmonary collaterals into the pulmonary circulation., As with TOF, the main role of imaging in patients with pulmonary, atresia and a VSD is assessment of postoperative complications. The most, common long-term complication is homograft failure: usually mixed, stenosis and regurgitation leading to RV dysfunction. Conduit stenosis is, often secondary to calcification of the non-viable homograft and although, calcified tissue is difficult to visualise using CMR, it is clearly seen on, CT. Other long-term complications are similar to those found in TOF., Key imaging goals, • Characterise the presence or absence of the central PAs., • Characterise the source of pulmonary blood flow (PDA or multifocal, MAPCAs)., • Quantify distance between RVOT and PA confluence., • Post-op (as for TOF): Assess RV-PA conduit function., , Aorta, , Ebstein’s, malformation, , Pulmonary artery, , Stenotic, pulmonary, valve, Fibrous tissue tags, A, , B, , Morphological LV, , VSD, Fibrous shelf, , Morphological RV, , Fig. 13.15 Congenitally Corrected Transposition of the Great Arteries. (A) Balanced steady-state freeprecession cardiac magnetic resonance image of congenitally corrected transposition of the great arteries, (CCTGA) showing the discordant atrioventricular connection with anterior left ventricle (LV). RV, Right ventricle., Note the apical offset of the left-sided tricuspid valve. (B) Schematic drawing of CCTGA and frequent associated, lesions. LV, Left ventricle; RV, right ventricle; VSD, ventricular septal defects., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 21 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , 309, , Pulmonary atresia with an intact ventricular septum. This is the, less common variant of pulmonary atresia. There is complete atresia, of the pulmonary valve in conjunction with a variable degree of, hypoplasia of the tricuspid valve and RV cavity. The type of surgical, repair depends on the size and shape of the RV cavity. The presence of, an RV infundibulum allows a biventricular repair. If the RV cavity is, small, then single ventricular physiology is established and angiography, demonstrates large venous sinusoids in the RV wall. Imaging assessment, is considered in the section below on the single ventricle., , Double Outlet Right Ventricle, The term double outlet right ventricle (DORV) refers to any cardiac, anomaly in which both the aorta and the pulmonary artery originate,, predominantly or entirely, from the right ventricle. In this situation the, LV has no direct outlet to either great vessel and must eject blood into, the RV through a VSD. Rarely there may be no VSD and then the LV, is very hypoplastic., The physiological picture and type of surgical correction depend, on the arrangement of the great vessels and the anatomy of the VSD., Cyanosis is not invariably present and depends on the degree of PS., The most common variant is a normal arrangement of the great vessels, and a subaortic VSD. This variant is often referred to as the ‘Fallot’s, type’ because it is often associated with PS and has a similar presentation., DORV may also be associated with an anterior aorta and a subpulmonary, VSD known as the ‘Taussig–Bing’ anomaly., Surgical correction for the ‘Fallot type’ variant consists of patch, closure of the VSD, which redirects blood to the aorta, and correction, of any PS. For the ‘Taussig–Bing’ anomaly the surgical approach depends, on the presence of pulmonary obstruction. In the absence of pulmonary, obstruction, correction consists of patch closure of the VSD and arterial, switch. In the presence of obstruction, LV flow is tunnelled through, the VSD to the aorta and an RV-PA pathway is established, known as, the Rastelli procedure., Imaging plays an important role in preoperative assessment. The, 3D anatomy of the VSD and the arrangement of the great vessels are, well visualised by CMR and are particularly important when deciding, the type of surgery. Black-bood spin-echo CMR of the VSD has been, shown to compare well with surgical findings and is able to indicate, the optimal type of repair., Key imaging goals, • Describe arrangement of great vessels—normal with subaortic, VSD (Fallot type), anterior aorta with subpulmonary VSD (Taussig–, Bing type)., • Describe VSD size, position and commitment., • Identify associated outflow tract obstruction., • Quantify shunt (may be left to right or right to left)., • Quantify ventricular volume, function and mass., • Postoperatively evaluate for TOF or TGA, described above, depending, on type of DORV., , Common Arterial Trunk, Common arterial trunk (truncus arteriosus) is defined as a single arterial, trunk arising from both ventricles, which overrides a large misaligned, VSD, Fig. 13.16. The pulmonary, systemic and coronary arteries all, originate from the trunk. This produces the physiological pattern of, cyanosis caused by intracardiac mixing as the simultaneous ejection of, both ventricles into the common trunk merges streams. The classification, of common arterial trunk relies on the branching pattern of the pulmonary artery. In type I, a short main pulmonary artery arises from, the common trunk and subsequently divides (see Fig. 13.16). In type, II, the right and left pulmonary arteries originate from the posterior, wall of the common trunk and, in type III, the right and left pulmonary, , Fig. 13.16 Unrepaired Truncus Arteriosus Presenting in a 17-Year-Old, Boy. A very short main pulmonary artery (MPA). Arises from the common, trunk before dividing into left and right pulmonary arteries. The patient, was cyanosed due to intracardiac mixing. There was pulmonary arterial, hypertension with an estimated pulmonary vascular resistance of 17, woods units.m2. VSD, Ventricular septal defect., , arteries emerge from the lateral wall of the common trunk. The truncal, valve is often abnormal, with varying degrees of stenosis and insufficiency., Approximately 40% of truncal arches are on the right side, with most, truncal arches rising higher in the mediastinum than the normal aortic, arch., Surgical repair consists of reconstruction of the common trunk to, produce a systemic vessel from the left ventricle, patch closure of the, VSD and establishment of a right ventricle-to-pulmonary artery conduit., The main role of CMR is in assessment of postoperative complications, (homograft failure, truncal valve regurgitation and VSD patch leak)., Imaging can be used to better delineate the vascular anatomy before, surgery., Key imaging goals, • Define morphological subtype:, • Type 1, RPA and LPA arise from a main PA segment., • Type 2, RPA and LPA arise from the posterior wall of the common, trunk., • Type 3, RPA and LPA arise from lateral wall of the common, trunk., • Describe truncal valve morphology (tricuspid, quadricuspid)., • Assess truncal valve function, stenosis or regurgitation., • Describe position of VSD., • Look for associated abnormalities, coarctation or interrupted, aortic arch., • If unrepaired, assess shunt and examine for pulmonary vascular, disease., , Anomalous Pulmonary Venous Connection/Drainage, Pulmonary veins may connect abnormally to a site other than the left, atrium—usually the right atrium, systemic vein or coronary sinus. If, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 22 : 310, , SECTION A The Chest and Cardiovascular System, , all the veins connect abnormally, then it is described as total anomalous, pulmonary venous connection/drainage (TAPVD), and if less than all, the veins connect abnormally (usually only 1) then it is termed partial, anomalous pulmonary venous connection/drainage (PAPVD). In TAPVD,, a complete left-to-right shunt causes all of the pulmonary venous return, to mix with systemic venous return. Survival is dependent on obligatory, right-to-left shunting of the mixed pulmonary venous and systemic, venous blood, usually at atrial level., PAPVD is an acyanotic condition, which results in a physiology, similar to an ASD. The number of veins involved determines the, magnitude of the shunt and the clinical symptoms. It is associated with, superior and inferior sinus venosus ASD (see Fig. 13.5C)., In TAPVD the pulmonary veins coalesce posterior to the left atrium, but do not drain into it. Drainage from this venous confluence to the, right atrium may be: (a) via either an ascending vein to the innominate, vein and then to the superior vena cava (SVC) (supracardiac, 50% of, patients, Fig. 13.17); (b) the coronary sinus directly into the right atrium, (cardiac, 15% of patients); (c) via a descending vein, which passes, , A, , through the diaphragm into either the IVC or portal venous system, (infracardiac, 25% of patients, Fig. 13.18); or (d) a mixture of these, routes may coexist (mixed, 10% of patients)., The infracardiac type is usually associated with a degree of obstruction as the descending vein passes through the diaphragm (see Fig., 13.18); thus, unlike the supracardiac and cardiac variants, which, present with a left-to-right shunt, intracardiac mixing and cardiac, failure, the clinical picture for infracardiac TAPVD is potentially more, severe, with superimposed pulmonary venous hypertension, resulting, in tachypnoea, tachycardia, liver enlargement, cyanosis, pulmonary, oedema and respiratory distress. Symptoms usually appear within 24, to 36 hours of birth. Importantly, the diagnosis of infracardiac TAPVD, can be missed on a ECG and must always be considered in the differential, diagnosis of pulmonary oedema on the neonatal chest radiograph, (see Fig. 13.18A)., Associations of TAPVD are complex cardiac anomalies such as, isomerism of the atrial appendages, AVSD, PS, DORV, hypoplastic, left-heart syndrome (HLHS), common arterial trunk, TGA and aortic, , B, , Fig. 13.17 Supracardiac Total Anomalous Pulmonary Venous Drainage. (A) Postero-anterior chest x-ray, in a teenager with a late presentation of supracardiac total anomalous pulmonary venous connection., (B) Volume-rendered gadolinium-enhanced magnetic resonance angiogram from the same patient. Note the, dilated superior vena cava (blue arrow) and right-sided pulmonary veins, which had evidence of obstruction., The patient subsequently underwent complete repair., , A, , B, , Fig. 13.18 Infracardiac Total Anomalous Pulmonary Venous Drainage. (A) Anterior-posterior chest x-ray, in newborn infant presenting with cyanosis and respiratory distress showing pulmonary oedema. (B) Volumerendered 3D reconstruction of magnetic resonance angiography showing total anomalous infracardiac drainage, of the pulmonary veins in the same patient. Note the narrowing of the veins as they pass through the diaphragm, (white arrow) before draining into the portal vein (blue arrow)., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 23 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, coarctation. The anomalous pulmonary venous connection is easily, visualised with ultrasound but in patients with poor ECG acoustic, windows, cross-sectional imaging with CMR and CT is very useful,, often avoiding the need for a diagnostic x-ray catheterisation., Key imaging goals, • Total anomalous pulmonary venous drainage:, • Describe pulmonary venous connection type: supracardiac, cardiac,, infracardiac or mixed., • Identify areas of pulmonary venous obstruction., • Confirm obligatory right-to-left shunt., • Identify associated abnormalities—isomerism of the atrial, appendage., • Partial anomalous pulmonary venous connection:, • Describe pulmonary venous connection., • Assess branch pulmonary arteries., • Quantify ventricular volume, function and assess RA dilatation., • Quantify shunt., • Consider if shunt measured but no ASD or VSD seen., • Consider PAPVC-associated conditions such as Turner’s syndrome., , SINGLE VENTRICLES, The term single ventricle covers a wide range of different cardiac, morphologies: for example, HLHS. (Fig. 13.19A), tricuspid atresia or, pulmonary atresia with intact ventricular septum; however, pragmatically,, the term can be used to describe a group of patients who, following, surgical ‘correction’, have a circulation supported by one ventricle., Modern palliative management has resulted in long-term survival for, many patients who would otherwise have died as infants., This division extends the narrower morphological classification to, include also functionally single ventricle: for example, where two, ventricles are connected by a large VSD, which cannot be surgically, septated because of AV valve apparatus straddling the ventricular septum, (chordae tendinae attached to the septal crest or opposite ventricle) or, when there is significant imbalance of the ventricular chambers, such, as in double inlet left ventricle., The ultimate management goal is the creation of a single ventricle, circuit with separation of the systemic and pulmonary circulations—a, Fontan or total cavopulmonary circulation (TCPC)—such that the single, ventricle pumps blood into the systemic circulation and systemic venous, return is directed to the pulmonary circulation without a ventricular, pump. This is performed in a step-wise surgical fashion involving two, or three stages., , Systemic to Pulmonary Artery Shunt, In patients with inadequate pulmonary blood flow caused by a hypoplastic, RV (tricuspid atresia or pulmonary atresia with intact ventricular septum), and in patients with HLHS as part of the Norwood procedure, the first, stage involves the creation of a systemic-to-pulmonary artery shunt, such as a modified BT shunt (see Fig. 13.13D). This is a temporising, procedure in infants, in whom PVR is not low enough to proceed, immediately with a bidirectional superior cavopulmonary connection, (BCPC), known as the Glenn procedure., Key imaging goals following stage 1: pre-bidirectional cavopulmonary connection (pre-BCPC), • Assess branch PA anatomy and exclude deformation at site of shunt, insertion., • In HLHS, assess aortic arch for residual obstruction or coarctation., • Assess systemic ventricular volume and function., • Identify any AV valve regurgitation., • Quantify aortic/neo-aortic valve regurgitation., • Evaluate adequacy of atrial communication., , •, •, , 311, , Look for systemic-pulmonary or veno-venous collateral vessels., Look for bilateral SVCs., , Bidirectional Glenn Circulation, The second stage in the creation of a single ventricular circulation is, the BCPC. It is usually performed at approximately 3 to 9 months of, age. In this procedure, an anastomosis is created between the SVC and, the right pulmonary artery (such that the SVC blood flows into both, arteries), and the SVC-RA junction oversewn (see Fig. 13.19B). Any, previous surgical systemic-to-pulmonary artery shunts are also taken, down at this time. Imaging should be used to assess branch pulmonary, artery narrowing and pulmonary venous obstruction; otherwise. The, circulation may fail., Key imaging goals following stage 2: pre-total cavopulmonary, connection (pre-TCPC), • Assess branch PA anatomy and SVC-PA connection., • Describe systemic venous return (SVC, IVC, hepatic veins)., • Quantify ventricular function and volume., • Identify AV valve regurgitation., • Describe outflow tracts and aortic arch., • Evaluate adequacy of atrial communication., • Look for veno-venous (usually SVC to IVC territory) or systemicto-pulmonary collateral vessels (common after BCPC) and quantify, collateral flow., • At time of general anaesthetic, assess pulmonary arterial pressure, by transducing the pressure in the internal jugular vein., • Look for pulmonary vein stenosis., , Fontan Circulation, The Fontan circulation can be completed by a number of different, surgical methodologies, but in the current era it is performed by the, creation of an intracardiac (lateral tunnel) (see Fig. 13.19C) or extracardiac conduit (Fig. 13.20A) between the IVC and the pulmonary, arteries. This is known as a total cavopulmonary connection (TCPC)., It is usually performed between 18 months and 5 years of age. The, classical Fontan operation involved connection of the SVC to the RPA, (non-bidirectional Glenn procedure) and connection of the right atrium, to the LPA (see Fig. 13.20B). Right atrial dilatation is the major complication of the classical Fontan procedure and may cause arrhythmias,, thrombosis or pulmonary vein compression, which can lead to failure, of the Fontan circulation. CMR allows evaluation of the branch pulmonary arteries and their systemic venous connections and can be used, to accurately assess ventricular function. Despite optimal medical and, surgical management, the intrinsic shortcomings of the TCPC invariably, manifest as late attrition during follow-up. This situation, known as a, ‘failing Fontan’, is particularly difficult to manage because systemic, venous hypertension and low cardiac output may result in peripheral, oedema and unusual clinical syndromes of plastic bronchitis and, protein-losing enteropathy (see Fig. 13.19D). Ultimately, this may result, in death or necessitate high-risk cardiac transplantation., Key imaging goals following stage 3: post-total cavopulmonary, connection (post-TCPC), • Assess branch PA anatomy and SVC-PA, IVC-PA connections. Exclude, stenosis., • Quantify ventricular volume and function., • Identify AV valve regurgitation., • Evaluate flow in fenestration between conduit and RA if present., • Evaluate adequacy of atrial communication., • Look for veno-venous or systemic-to-pulmonary collateral vessels, (common after BCPC) and quantify collateral flow., • Look for thrombus in RA if classical Fontan., • Identify any pulmonary vein stenosis., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 24 : 312, , SECTION A The Chest and Cardiovascular System, , A, , B, , C, , D, Fig. 13.19 Single Ventricle. (A) Balanced steady-state free-precession (b-SSFP) cardiac magnetic resonance, (CMR) image showing hypoplastic left heart syndrome, with severe hypertrophy of the systemic right ventricle, (RV). LV, Left ventricle. Note the large interatrial communication (arrowed) that allows mixing of systemic, and pulmonary venous return. (B) Volume-rendered 3D reconstruction of a magnetic resonance angiogram, showing the Glenn, bidirectional cavopulmonary anastomosis (arrow) and (C) a lateral tunnel total cavopulmonary, anastomosis (arrow) to the right pulmonary artery (arrowhead). (D) b-SSFP CMR image showing severe, ascites (arrow) and right pleural effusion (arrowhead) in a patient with a failing total caval pulmonary connection, circulation and protein-losing enteropathy., , Recent Developments in Cardiac Magnetic, Resonance Imaging, Hybrid Catheter/Cardiac Magnetic Resonance, Imaging Laboratory, , In a hybrid catheter/CMR lab (XMR), a cardiac catheterisation laboratory is connected to the CMR scanner via a shielded sliding door., , A mobile patient table facilitates seamless transfer between the two, techniques., As a diagnostic tool, XMR is particularly helpful in the evaluation of haemodynamic problems in which pressure-only or flow-only, measurements result in an incomplete characterisation of the problem:, for example. In the assessment of PVR for pulmonary hypertension. XMR, can also be used to guide structural intervention and electrophysiological, , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 25 : CHAPTER 13 Congenital Heart Disease: General Principles and Imaging, , 313, , B, , A, , Fig. 13.20 (A) Total cavopulmonary connection using an extracardiac conduit from the IVC to the pulmonary, arteries in a patient with hypoplastic right heart caused by pulmonary atresia and intact ventricular septum., (B) Volume-rendered magnetic resonance angiogram of atriopulmonary Fontan in a patient with tricuspid, atresia. Note the anastomosis between the right atrial appendage and the main pulmonary artery, MPA, (blue, arrow). CS, coronary sinus; IVC, inferior vena cava; LPA, left pulmonary artery; RA, right atrium; RPA, right, pulmonary artery; SVC, superior vena cava., , studies and in these cases would reduce the radiation exposure, which, is particularly important in children and infants., , Fetal Cardiac Magnetic Resonance Imaging, Fetal CMR is an emerging technique that may prove complementary, to a fetal ECG. As with other ultrasound techniques, a fetal ECG can, be affected by maternal body habitus or other situations that reduce, acoustic windows. Fetal CMR is affected by several technical challenges, related to the fetal cardiac dimensions and fast heart rate, fetal motion, and the lack of fetal ECG trace for gating., , Post-Mortem Cardiac Magnetic Resonance Imaging, Perinatal and paediatric cardiac autopsies have an important role in, the counselling of parents with regard to the cause and implications, of death of their child. Recently, less invasive post-mortem MR has, been proposed as an alternative for conventional autopsy and could be, used as the first-line assessment for structural heart disease in this situation. Post-mortem imaging allows an opportunity to investigate the, heart in situ before dissection and both post-mortem CT and postmortem MRI have shown excellent accuracy in detecting most clinically, significant cardiac lesions in the perinatal and paediatric population., If all non-diagnostic and positive post-mortem CMR scans were referred, for conventional autopsy, very few diagnoses would be missed based, upon currently available evidence., , Three-Dimensional Printing, Three-dimensional-engineered replicas of different anatomical structures, have been used extensively in different fields of medicine over the past, 20 years. As the manufacturing techniques, referred to as ‘rapid prototyping’, have become more refined over the years, medical researchers, , have used such 3D models for pre-surgical planning personalisation, of prostheses or testing of novel devices. One of the other benefits, of anatomical 3D models is being able to visualise the location and, dimensions of the area of interest as an aid in communication, both, within a surgical team and, crucially, between the physician and, the patient., Any 3D cardiac images (CMR, CT or echo) can be used to create a, 3D model. The 3D data needs to be extracted from the images and, then converted into an .stl file that can be input into a 3D printer. The, 3D piece can be manufactured using a wide variety of materials to meet, the needs of the model—rigid for patient explanation, flexible for device, pre-procedural planning and tissue-like for surgical practice with suturing, (Fig. 13.21)., , CONCLUSION, CHD is a complex area of medicine that requires a well-integrated, understanding of anatomy and cardiovascular physiology. Using the, principles illustrated in this chapter, cardiovascular imaging can be, successfully utilised to guide medical and surgical management of patients, with CHD. An ECG remains the first-line imaging technique; however,, when an ECG cannot provide a complete diagnosis, cross-sectional, imaging with CMR and CT is the next line of investigation. Catheter, angiography is usually reserved for problem solving, coronary artery, assessment, haemodynamics and for catheter-guided therapeutic, procedures., It is hoped that the complementary nature of imaging techniques, has been demonstrated and that when used in combination, ECG, CMR,, CT and x-ray catheter angiography can provide a comprehensive, assessment of patients with CHD., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.
Page 26 : 314, , SECTION A The Chest and Cardiovascular System, , A, , B, , C, , D, , Fig. 13.21 Three-Dimensional Printing of a Variety of Congenital Anatomies Made From Different, Materials. (A) Great vessels in rigid material for patient education. (B) Multicolour print: right heart printed, in purple, left heart in red. (C) Transparent material for visualisation of device deployment in coarctation. (D), Right ventricular outflow tract and pulmonary trunk for testing deployment of novel pulmonary valve device., , FURTHER READING, Anderson, R., Baker, J., Penny, D., et al., 2010. Paediatric Cardiology, third ed., Churchill Livingstone, Edinburgh., Bogaert, J., Dymarkowski, S., Taylor, A., et al., 2012. Clinical Cardiac MRI., Springer, New York., Han, B.K., Rigsby, C.K., Hlavacek, A., et al., 2015. Computed tomography, imaging in patients with congenital heart disease part I: rationale and, utility. An expert consensus document of the Society of Cardiovascular, Computed Tomography (SCCT): endorsed by the Society of Pediatric, Radiology (SPR) and the North American Society of Cardiac Imaging, (NASCI). J. Cardiovasc. Comput. Tomogr. 9, 475–492., , Han, B.K., Rigsby, C.K., Leipsic, J., et al., 2015. Computed tomography, imaging in patients with congenital heart disease, part 2: technical, recommendations. An expert consensus document of the Society, of Cardiovascular Computed Tomography (SCCT): endorsed by the, Society of Pediatric Radiology (SPR) and the North American Society, of Cardiac Imaging (NASCI). J. Cardiovasc. Comput. Tomogr. 9,, 493–513., Lai, W.W., Mertens, L., Cohen, M., et al., 2009. Echocardiography in Pediatric, and Congenital Heart Disease: From Fetus to Adult. Wiley-Blackwell,, Oxford., Sridharan, S., Price, G., Tann, O., et al., 2010. Cardiovascular MRI in, Congenital Heart Disease: An Imaging Atlas. Springer, Berlin; London., , Downloaded for Abhishek Srivastava (
[email protected]) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on January 11, 2022. For personal use only. No other uses without permission. Copyright ©2022. Elsevier Inc. All rights reserved.