Page 1 :
Heart, Lung and Circulation (2020) 29, 772–779, 1443-9506/04/$36.00, https://doi.org/10.1016/j.hlc.2019.01.019, , ORIGINAL ARTICLE, , Surgical Outcomes of Anatomical Repair, for Congenitally Corrected Transposed, Great Arteries, Kai Ma, MD, PhD, Lei Qi, MD, Zhongdong Hua, MD, Keming Yang, MD,, Hao Zhang, MD, PhD, Shoujun Li, MD *, Sen Zhang, MD, PhD,, Fengpu He, MD, Guanxi Wang, MD, Zicong Feng, MD, Pediatric Cardiac Surgery Center, National Center for Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences, Peking Union, Medical College, Beijing, PR China, Received 11 November 2017; received in revised form 14 January 2019; accepted 28 January 2019; online published-ahead-of-print 26 April 2019, , Background, , The outcomes of anatomical repair for patients with congenitally corrected transposed great arteries remain, unclear and the indications for different procedures are poorly understood., , Methods, , From January 2005 to February 2016, consecutive corrected transposition patients who underwent anatomical repair at the current institution were enrolled in this retrospective study. Varied types of anatomical, repair were individually customised., , Results, , A total of 85 patients were included. Fifty-one (51) and 35 patients presented with left ventricular outflow, tract obstruction and cardiac malposition, respectively. Thirty-nine (39) patients presented with moderateto-severe tricuspid regurgitation. Thirty-four (34), 19, and 32 patients underwent Senning arterial switch, operations, Senning-Rastelli, and hemi-Mustard-Rastelli-bidirectional Glenn, respectively. Early after, repair, there were five in-hospital deaths and nine re-operations. During 4.6 years (range, 0.5–10.3) of, follow-up, seven late deaths were documented. Estimated overall survival rate after anatomical repair, was 89.3%, 85.0%, and 85.0% at 1 year, 3 years, and 5 years, respectively. Instead of Senning-Rastelli, most, (75.0%) early left ventricular dysfunctions were noted in patients who underwent Senning arterial switch, procedures. However, all the late left ventricular dysfunctions were found in patients who underwent, previous left ventricular retraining. In patients with left ventricular outflow tract obstruction, the hemiMustard-Rastelli-bidirectional Glenn shunt provided a lower early mortality (0% vs 15.8%, p = 0.047)., , Conclusions, , Favourable outcomes can be achieved for anatomical repair of corrected transposition. Left ventricular, dysfunction was a significant postoperative issue. Hemi-Mustard-bidirectional Glenn-Rastelli procedure, may provide benefits for patients with associated left ventricular outflow tract obstruction and cardiac, malposition. Each procedure has its own advantages in varied anatomy., , Keywords, , Congenital heart disease � Cardiac surgery � Corrected transposition of the great arteries � Anatomical, repair, , *Corresponding author at: Department of Cardiac Surgery, Fuwai Hospital, CAMS & PUMC, 167 Beilishi Road, Xicheng District, Beijing, 100037, People’s, Republic of China. Tel.: +86(10)88398855; Fax: +86(10)88398855., Email: drlishoujun@yahoo.com, © 2019 Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) and the Cardiac Society of Australia and New Zealand (CSANZ)., Published by Elsevier B.V. All rights reserved., , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 2 :
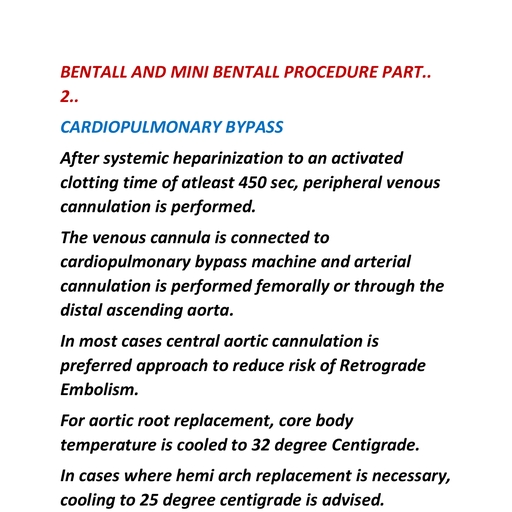
Anatomical Repair for Congenitally Corrected Transposed Great Arteries, , Introduction, Congenitally corrected transposition of the great arteries, (ccTGA) is characterised by a combination of atrioventricular, and ventriculoarterial discordance. Morphologic left ventricle (LV) and right ventricle (RV) support the pulmonary and, systemic circulations, respectively [1]. The lesions most commonly associated with ccTGA (e.g., ventricular septal defect, (VSD), left ventricular outflow tract obstruction (LVOTO),, and cardiac positional anomalies) are considered to be significant factors when customising surgical procedures [2]., Key breakthroughs in the practice of arterial switch operations (ASO) – Rastelli, Senning and Mustard procedures for, transposition of the great arteries – have resulted in a prevalence of double switch (Senning-ASO and Senning-Rastelli),, which restores the LV to systemic circulation and is considered to be an anatomical correction [3,4]. However, complex, anatomy, including dextrocardia or mesocardia, can greatly, affect creation of an atrial baffle in the Senning procedure., Furthermore, development of LV (systemic ventricle) dysfunction late after double switch remains a concern, particularly in patients with previous morphologic LV retraining [5]., Multiple benefits of the hemi-Mustard-Rastelli-bidirectional, Glenn shunt (BDG) procedure for ccTGA patients with LVOTO, have been demonstrated since it was introduced by Malhotra, et al. [6,7]. One of the most important advantages of the hemiMustard approach compared with conventional atrial baffle, procedures is the relatively simple technique when rerouting, blood from the vena cava to the tricuspid valve [7]. This, approach is not only technically feasible but has favourable, outcomes when cardiac malposition presents [8]., The aim of this study was to report the results of anatomical repair for ccTGA and to determine the individual customisation of varied surgical approaches achieving anatomical, repair., , Patients and Methods, Patients, From January 2005 to February 2016, consecutive ccTGA, patients who underwent anatomical repair at the current, institution were enrolled into this retrospective study., Anomalous pulmonary venous connection, atrioventricular, septal defect, remote VSD (unrouteable), unbalanced ventricles, heterotaxy syndrome, and univentricular physiology, were considered to be contraindications for anatomical, repair. Patients who were put into the single ventricular, palliation track (with total cavopulmonary connection as a, surgical route) were excluded. This study was approved by, the Ethics Committee at Fuwai Hospital. They granted, approval to waive the need for patient consent for publishing, follow-up data on these patients., , Endpoints, The primary endpoint was postoperative death, including, early and late death. Secondary endpoints were moderate or, , 773, , severe postoperative LV dysfunction and a composite endpoint of death and or New York Heart Association III or IV at, the last follow-up. Early death or LV dysfunction was, defined as occurring within 30 days of surgery. Late death, or LV dysfunction was defined as occurring >30 days after, surgery. Ventricular dysfunction was defined as an ejection, fraction <50% measured by echocardiography., , Surgical Strategy, Indications for varied approaches of anatomic repair, depended on anatomic features. Mild tricuspid regurgitation, (TR) was considered as the timing for surgical intervention in, patients without significant LVOTO. When cyanosis or, abnormal pulse oximeter oxygen saturation (SO2) presented,, surgery was indicated in patients with significant LVOTO., At the arterial level, the Rastelli procedure was performed, in patients with significant LVOTO, connecting the VSD to, the aorta via an intraventricular baffle, and the RV to the, pulmonary artery via an extracardiac conduit. An ASO was, the prevalent approach for patients who had an unobstructed, LV outflow tract. At the atrial level, the Senning procedure, was the surgical choice for patients with normal cardiac, position. Before 2012, the hemi-Mustard procedure was, not performed at the current institution. Hence, the Senning, procedure was also performed when cardiac malposition, presented. Hemi-Mustard-BDG was indicated in patients, with cardiac malposition after 2012. As shown in Figure 1,, various types of procedures were individually customised., Pulmonary artery banding and a modified Blalock-Taussig, shunt were previously used as palliative approaches to, restrict pulmonary blood flow, retrain the morphologic, LV, and alleviate cyanosis. Concomitant to anatomical repair,, tricuspid valvuloplasty was performed when more than mild, TR was present., , Surgical Techniques, As previously published [9], median sternotomy, cardiopulmonary bypass, and cold blood cardioplegia were used in, Senning-ASO or Senning-Rastelli and the hemi-MustardRastelli-BDG procedures., Senning-Arterial Switch Operation or Senning-Rastelli, A VSD repair was transatrially performed through the, aorta or RV. Shumacker modification of the Senning procedure, utilising in situ pericardium to complete the pulmonary venous atrium, was always used. The Lecompte, manoeuvre was generally performed if the great arteries, were not located side by side. Plication of the neo-aorta, wall at the sinotubular junction was performed to avoid, root dilation., Hemi-Mustard, Rastelli or Bidirectional Glenn, The hemi-Mustard procedure was performed after the aorta was, clamped: the atrial septum was completely excised; the coronary, sinus was unroofed; and a bovine pericardial baffle was constructed to divert blood flow from the inferior vena cava (including the left superior vena cava if present) and a coronary sinus to, the tricuspid valve. For the Rastelli procedure, an extracardiac, , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 3 :
774, , K. Ma et al., , Figure 1 Relationship between anatomical features and surgical procedures., Abbreviations: CCTGA, congenitally corrected transposition of the great arteries; LVOTO, left ventricular outflow tract, obstruction; SO2, oxygen saturation; VSD, ventricular septal defect; LV, left ventricle; DS, double switch; PAB-T, pulmonary, arterial banding for LV retraining; PAB-P, pulmonary arterial banding reducing pulmonary blood; BDG, bidirectional Glenn, shunt; B-T shunt, Blalock-Taussig shunt., , conduit was established with caution so that sternal compression could be avoided. The BDG was usually performed after, removal of the aortic cross-clamp., , Data Collection and Definition, Medical records, preoperative and postoperative records,, images, and operative notes were obtained from a local, database and reviewed. The degree of valve regurgitation, was graded from 0–4 using Sellers’ classification, and was, numerically expressed as: 0, absent and trivial; 1, mild;, 2, moderate; and 3, severe [10]. Valvular regurgitation was, considered significant when documented as moderate or, severe, and LVOTO was considered significant when the, systolic pressure gradient was �70 mmHg or pulmonary, valvular morphologic anomalies presented. Ventricular dysfunction was graded as mild (40%� ejection fraction (EF), <50%), moderate (30%� EF < 40%) and severe (EF < 30%)., Ventricular dysfunction was considered significant when, documented as moderate or severe. Pulmonary arterial, hypertension was defined as mean pulmonary artery pressure �25 mm Hg., , Statistical Analysis, Comparisons of variables were made using the Student’s, t-test, analysis of variance (ANOVA), Chi-square test, or, Fisher’s exact test. Time to death and time to postoperative, LV dysfunction were displayed by Kaplan-Meier curves., Logistic regression (forward) was performed as multivariate, analysis to investigate risk factors for death. The level of, significance was set at an alpha level of �0.05. Analysis, was conducted using SPSS version 19.0 (IBM-SPSS Inc,, Armonk, NY, USA) for Windows., , Results, Patient Population and Anatomic, Characteristics, From January 2005 to February 2016, 85 consecutive patients, with ccTGA and two adequately sized ventricles underwent, anatomical repair at the current institution. The median age, and weight at anatomical repair were 4.8 years (range, 8, months to 12 years) and 12.2 kg (range, 7.1–24.4 kg), respectively. Tricuspid regurgitation was present in 61 (71.7%), patients, including 22 (25.9%) mild, 18 (21.2%) moderate,, and 21 (24.7%) severe., Fifty-one (51) (60.0%) patients had a significant LVOTO,, comprising 44 (51.8%) pulmonary stenosis and seven (8.2%), pulmonary atresia. Mesocardia and dextrocardia presented, in 10 (11.8%) and 25 (29.4%) patients, respectively. Unrestrictive VSD was the most common associated cardiac defect and, presented in 40 (47.1%) patients. Among patients who had, unrestrictive VSD, 10 (11.8%) significant pulmonary vascular, obstructive disease (PVOD) were confirmed by catheter., Fifteen (15) (17.6%) patients co-presented with persistent left, superior vena cava and two (2.35%) patients required preoperative permanent pacing for spontaneously complete, heart block. Associated anomalies in each surgical group, are listed in Table 1., , Surgical Procedures, Fourteen (14) of 85 patients (16.5%) had a palliative shunt before, anatomical repair, including three (2.7%) modified BlalockTaussig shunts and 11 BDG. Pulmonary artery banding, (PAB) was used as an interim measure to either prevent, , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 4 :
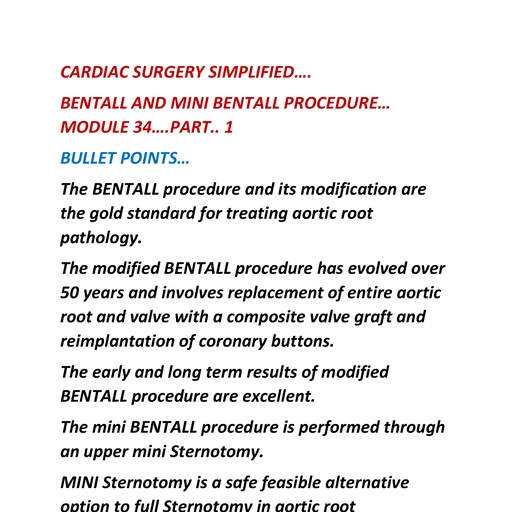
775, , Anatomical Repair for Congenitally Corrected Transposed Great Arteries, , Table 1 Patients’ characteristics., Senning-ASO, , Senning-Rastelli, , Hemi-Mustard-Rastelli-BDG, , N = 34, , N = 19, , N = 32, , Median age at anatomical repair, years, , 3.1, , 4.0, , 5.4, , At least mild TR, , 34 (100.0%), , 10 (52.6%), , 17 (53.1%), , Mild, , 15 (44.1%), , 2 (10.5%), , 5 (15.6%), , Moderate, , 11 (32.3%), , 3 (15.8%), , 4 (12.5%), , Severe, , 8 (23.5%), , 5 (26.3%), , 8 (25.0%), , Associated anomalies, Cardiac malposition, , 3 (8.8%), , 0, , 32 (100.0%), , LVOTO, Unrestrictive VSD, , 0, 12 (35.3%), , 19 (100.0%), 19 (100.0%), , 32 (100.0%), 32 (100.0%), , Persistent left superior vena cava, , 9 (26.5%), , 1 (5.3%), , 7 (21.9%), , PVOD, , 10 (29.4%), , 0, , 0, , Tricuspid valve abnormalities, , 6 (17.6%), , 3 (15.8%), , 5 (15.6%), , Palliative surgery, Pulmonary arterial banding, , 21 (61.8%), , 0, , 0, , Modified B-T shunt, , 0, , 3 (15.8%), , 0, , Bidirectional Glenn shunt, , 0, , 0, , 11 (34.4%), , Abbreviations: ASO, arterial switch operation; BDG, bidirectional Glenn shunt; TR, tricuspid regurgitation; LVOTO, left ventricular outflow tract obstruction; VSD, , ventricular septal defect; PVOD, pulmonary vascular obstructive disease; B-T shunt, Blalock-Taussig shunt., , pulmonary hypertension (PAB-protection, n = 1) or train the, morphologic LV (PAB-training, n = 20). None of the patients, in the whole cohort required more than one palliative procedure., Eighty-five (85) anatomical repair approaches were performed, including: (1) Senning-ASO (n = 34, 40.0%); (2), Senning-Rastelli (n = 19, 22.4%); and (3) hemi-Mustard-Rastelli-BDG (n = 32, 37.6%). Among the three surgical procedures, there was no significant between-approach difference, for both cardiopulmonary bypass time (ANOVA, p = 0.332), and cross-clamp time (ANOVA, p = 0.472). Concomitant procedures included 52 (61.2%) tricuspid repairs, 10 (11.8%), mitral repairs, four (4.7%) VSD enlargements, 11 (12.9%), pulmonary angioplasties, two (2.4%) aortic repairs, and five, (5.9%) pacemaker implantations., Among the 51 Rastelli approaches, RV to pulmonary artery, conduit was addressed by bovine jugular vein conduit. Both, the VSD closure and the intraventricular baffle were established by Dacron patch in all patients. Three patients who, had positional cardiac anomalies (but not LVOTO) before, 2012 underwent Senning-Rastelli procedures. Two extracorporeal membrane oxygenation (ECMO) supports were, required. Twenty-seven patients who underwent BDG, (84.4%) had concomitant ligation of the azygous vein., , Mortality, Early after repair, there were five (5.9%) in-hospital deaths within, the year of surgery before 2012 (HR, 3.2; p = 0.020; 95% CI, 1.2–5.0), identified as the only risk factor in multivariate analysis. Cause of, early deaths included low cardiac output syndrome (three of five,, 60.0%), respiratory infection (one of five, 20.0%), and inability, weaning off ECMO support (one of five, 20.0%)., , There was no patient lost during a 4.6-year (range, 0.5 to, 10.3) follow-up. Seven (7) (8.8%) follow-up deaths were, documented. Estimated overall survival rate after anatomical repair was 89.3%, 85.0%, and 85.0% at 1 year, 3 years, and, 5 years, respectively (Figure 2). Left ventricular dysfunction, contributed to the majority of follow-up deaths (five of, seven, 71.4%). Mortality in each surgical group is shown, in Table 2., , Morbidity, Three patients (one Senning-ASO, two Senning-Rastelli, and, no hemi-Mustard-Rastelli-BDG) required postoperative, ECMO support. Two of them were successfully weaned from, it. The other patient required ECMO for coronary kinking,, failed to recover, and died. There were nine (10.6%) early reoperations documented. The most common early complication was complete heart block (four of 85, 4.7%) requiring, implantation of a permanent pacemaker. In the whole cohort,, five (5.9%) atrial baffles were revised for venous drainage, obstruction. During the follow-up period, no patients, required transplantation. Two (2.7%) RV-PA conduits and, two (2.7%) intra-atrial baffles (one baffle stenosis and one, baffle leak) were replaced and revised, respectively. In, patients who underwent Senning-ASO, three (10.7%) severe, neo-aortic regurgitations were documented. No survivors, had coronary complications during follow-up., , Tricuspid Regurgitation, The degree of TR significantly improved after anatomical, repair (1.42 � 1.15 vs 0.42 � 0.67, p < 0.001) (as shown in, Table 3)., , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 5 :
776, , K. Ma et al., , Figure 2 Estimated survival and freedom from re-operation., A: Estimated survival., B: Freedom from moderate-to-severe left ventricular dysfunction among survivors., , Table 2 Early and follow-up outcomes., Senning-ASO, , Senning-Rastelli, , Hemi-Mustard-Rastelli-BDG, , N = 34, , N = 19, , N = 32, , Early deaths, , 2 (5.9%), , 3 (15.8%), , 0, , Early moderate-to-severe LV dysfunction, , 3 (8.8%), , 1 (5.3%), , 0, , ECMO support, , 1 (2.9%), , 2 (10.5%), , 0, , Early re-operation, , 4 (11.8%), , 1 (5.3%), , 4 (12.5%), , Pacemaker implantation, , 1 (2.9%), , 0, , 3 (9.4%), , Atrial baffle revision, , 3 (8.8%), , 1 (5.3%), , 1 (3.1%), , 1 (2.9%), , 0, , 0, , Early outcomes, , Coronary kinking, Follow-up outcomes, Follow-up deaths, , 5 (15.6%), , 1 (6.3%), , 1 (3.1%), , Late moderate-to-severe LV dysfunction, , 2 (7.4%), , 0, , 0, , Transplantation, , 0, , 0, , 0, , Extra-cardiac conduit replacement, , 0, , 2 (13.3%), , 0, , Venous drainage obstruction, , 1 (3.7%), , 1 (6.3%), , 0, , NYHA III-IV, , 4 (14.8%), , 4 (26.7%), , 5 (16.1%), , SO2 at follow-up, Severe neo-aortic regurgitation, , 98.3 � 2.9%, 3 (11.1%), , 96.1 � 3.5%, 0, , 90.2 � 3.7%, 0, , 11 (32.4%), , 8 (42.1%), , 6 (18.8%), , Overall death and NYHA III or IV at follow-up, , Abbreviations: ASO, arterial switch operation; BDG, bidirectional Glenn shunt; LV, left ventricle; ECMO, extracorporeal membrane oxygenation; NYHA, New, York Heart Association functional classes; SO2, oxygen saturation., , Functional Status, At the latest follow-up, there were 13 (17.8%) patients in, NYHA functional class III-IV. The SO2 of patients who, had, hemi-Mustard-Rastelli-BDG, procedures, was, 90.2 � 3.7%, which was not significantly lower when compared with patients who underwent Senning-ASO, , (98.3 � 2.9%, p = 0.272) and those who underwent SenningRastelli (96.1 � 3.5%, p = 0.505) procedures., , Systemic Left Ventricular Dysfunction, Instead of Senning-Rastelli, most (three of four, 75.0%) early, significant LV dysfunctions were noted in patients who, , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 6 :
777, , Anatomical Repair for Congenitally Corrected Transposed Great Arteries, , Table 3 Changes in tricuspid regurgitation after anatomical repair., Absent or Trivial, , Mild, , Moderate, , Severe, , 10 (29.4%), , 8 (23.5%), , 7 (20.6%), , 9 (26.5%), , 23 (71.8%), , 5 (15.6%), , 3 (9.4%), , 1 (3.1%), , Preoperative (n = 19), , 5 (26.3%), , 4 (21.1%), , 4 (21.1%), , 6 (31.6%), , Postoperative (n = 16), , 12 (75.0%), , 3 (18.8%), , 1 (6.3%), , 0, , Preoperative (n = 32), , 9 (28.1%), , 10 (31.3%), , 7 (21.9%), , 6 (18.8%), , Postoperative (n = 32), , 18 (56.2%), , 13 (40.6%), , 1 (3.1%), , 0, , Senning-ASO, Preoperative (n = 34), Postoperative (n = 32), , P-value, 0.003, , 0.004, , Senning-Rastelli, , 0.001, , Hemi-Mustard-Rastelli-BDG, , Abbreviations: ASO, arterial switch operation; BDG, bidirectional Glenn shunt., , underwent Senning-ASO procedures. However, the two, (2.7%) late significant LV dysfunctions were found in, patients who underwent previous morphologic LV retraining. On multivariate analysis, previous LV retraining (HR,, 4.7; p = 0.003; 95% CI, 2.1–6.2) was an independent risk factor, for overall significant LV dysfunction. Estimated freedom, from significant LV dysfunction after anatomical repair was, 95.0%, 91.7%, and 91.7% in 1 year, 3 years, and 5 years,, respectively (Figure 2)., , Outcomes of Patients who had Cardiac, Positional Anomalies, Since 2012, the hemi-Mustard-Rastelli-BDG procedure was, routinely performed in patients with cardiac malposition and, LVOTO. Hence, a cohort of patients with cardiac positional, abnormalities was spontaneously generated, consisting of, three patients who underwent Senning-ASO (no LVOTO), and 32 who underwent hemi-Mustard-Rastelli-BDG (with, LVOTO)., As Table 4 shows, there was more significant early LV, dysfunction (three of three, 100.0% vs 0 of 32, 0%) and more, early deaths (two of three, 66.7% vs 0 of 32, 0%) in patients who, had Senning-ASO. Furthermore, the follow-up mortality was, much lower in patients with hemi-Mustard-Rastelli-BDG (one, of 32, 3.1% vs one of one, 100.0%)., , Outcomes of Patients who had Left, Ventricular Outflow Tract Obstruction, On analysis, when comparing between-procedure outcomes, of patients associated with LVOTO, it was found that lower, early mortality was documented in patients who had hemiMustard-Rastelli-BDG than Senning-Rastelli procedure (0%, vs 15.8%, p = 0.047), despite a higher incidence of positional, anomalies. Moreover, SO2 (91.2 � 3.0% vs 96.3 � 2.2%,, p = 0.482) and NYHA functional class III-VI (16.1% vs, 26.7%, p = 0.445) at the latest follow-up were similar (shown, in Table 5)., , Discussion, From January 2005 to February 2016, 85 patients with ccTGA, underwent anatomical repair at Fuwai Hospital. This study, analysed data on this relatively large cohort, with a focus on, surgical strategy. This study confirmed that an anatomical, repair can be achieved with favourable outcomes in the, majority of patients with ccTGA., Varied surgical approaches were performed for anatomical repair (Figure 1). Presence of LVOTO, cardiac positional, anomalies, and unrestrictive VSD were determinants of surgical strategy, and obtained favourable outcomes. Consistent, , Table 4 Outcomes of patients who had cardiac malposition., Senning-ASO N = 3, , Hemi-Mustard-Rastelli-BDG N = 32, , P-value, , Early moderate-to-severe LV dysfunction, , 3 (100.0%), , 0, , <0.001, , Early reoperation, , 1 (33.3%), , 4 (12.5%), , 0.380, , Early death, , 2 (66.7%), , 0, , 0.005, , Late death, , 1 (100.0%), , 1 (3.1%), , 0.061, , NYHA class III-IV at follow-up, SO2 at follow-up, , NA, NA, , 5 (16.1%), 91.2 � 3.0%, , NA, NA, , Abbreviations: ASO, arterial switch operation; BDG, bidirectional Glenn shunt; LV, left ventricle; NYHA, New York Heart Association functional classes; SO2,, oxygen saturation., , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.
Page 7 :
778, , K. Ma et al., , Table 5 Outcomes of patients who had left ventricular outflow tract obstruction., Senning-Rastelli group N = 19, , Hemi-Mustard-Rastelli-BDG group N = 32, , P-value, , LV significant dysfunction, Early re-operation, , 1 (5.2%), 2 (10.5%), , 0, 4 (12.5%), , 0.373, >0.999, , Early death, , 3 (15.8%), , 0, , 0.047, , Late death, , 1 (6.3%), , 1 (3.1%), , >0.999, , Extra-cardiac conduit replacement, , 2 (13.3%), , 0, , 0.101, , NYHA class III-IV at follow-up, , 4 (26.7%), , 5 (16.1%), , 0.445, , SO2 at follow-up, , 96.3 � 2.2%, , 91.2 � 3.0%, , 0.482, , Abbreviations: BDG, bidirectional Glenn shunt; LV, left ventricle; NYHA, New York Heart Association functional classes; SO2, oxygen saturation., , with previously published reports [12,13], double switch, (Senning-ASO and Senning-Rastelli) remained the prevailing, procedure for anatomical repair of ccTGA [11,12,13]., Both short-term and long-term survival in this series, favourably compared with other series [14,15]. Accompanying surgical techniques have improved in the last decade,, and a growing proportion of patients are surviving complex, anatomical repair. In the current multivariate analysis, the, only risk factor for early death was time of surgery before, 2012, suggesting more mature surgical techniques and, appropriate perioperative management in the current era., In 2003, Langley et al. reported a cohort with a postoperative, survival of 94.4 � 3.1% at 1 year and 89.7 � 4.4% at 9 years, [16]. More recently, Murtuza et al. reported that survival in, patients who underwent Senning-ASO was 83.9% at 5 years,, and 91.6% in patients who underwent Senning-Rastelli [17]., The trend that long-term mortality after Senning-Rastelli is, lower than Senning-ASO was also noticed in the current, study (15.6% vs 6.3%)., The majority (71.4%) of follow-up deaths were caused by, morphologic LV dysfunction in the current cohort. Furthermore, six postoperative morphologic LV dysfunctions were, documented. Murtuza et al. reported that 23.5% of patients, who underwent Senning-ASO developed follow-up LV dysfunction, and they found that ccTGA patients with LVOTO, had more favourable longer-term outcomes than those without LVOTO [17]. Sharma et al. also stated that 12.5% of, survivors after Senning-Rastelli procedure had LV dysfunction [18]. Murtuza et al. reported deterioration in LV function, in the trained group of patients after anatomic repair (39% of, patients who had impaired LV function) [19]. In a previous, study that focussed on two-stage Senning-ASO, 60% of late, deaths in patients who had LV retraining were attributed to, poor LV performance [5]., Myers et al. reported their experience in using PABtraining for retraining the LV in ccTGA. Late LV dysfunction was significantly more frequent in older patients, both, at PAB and anatomic repair, with cut-off values of ages 2, years and 3 years, respectively [20]. In fact, the referral was, late and the age at PAB-training was much higher in the, current patients, which contributed to poor LV function., Although Sharma et al. concluded that less-aggressive, , banding techniques are associated with decreases in morphologic LV function after double switch [21], there is, ongoing controversy about these techniques., In the current cohort, there was no morphologic LV dysfunction after hemi-Mustard-Rastelli-BDG procedure, which, subsequently improved overall survival. In 2012, Sojak et al., stated that LV function was preserved in all their patients, when using hemi-Mustard and BDG approaches [7]. The, ground-breaking article by Malhotra et al. also confirmed, that there was no postoperative LV dysfunction in patients, who had LVOTO and underwent hemi-Mustard-RastelliBDG [6]., However, the mechanism of LV function preservation after, anatomical repair remains unclear and largely uninvestigated. Bautista-Hernandez revealed that univentricular, (dual-chamber) pacing was a significant risk factor for, post-anatomical repair dysfunction, whereas biventricular, pacing appeared to preserve systemic ventricular function, [22]. This study suggested that ventricular dyssynchrony, plays an important role in the functional deterioration of, the systemic ventricle in patients with ccTGA, which was, confirmed by Hofferberth et al. [23]., At the current institution, the hemi-Mustard-RastelliBDG procedure is indicated when the patient presents with, dextrocardia or mesocardia because the technical simplicity, of the hemi-Mustard procedure can significantly reduce, cross-clamp time and provide a lower incidence of postoperative venous drainage obstruction. Obstructive venous, return created by the Senning procedures has been reported, in 5–7% of cases [24–26], and is much more common in, patients with cardiac malposition. In the current study, one, intra-atrial baffle obstruction was seen after hemi-Mustard, procedure. One of the potential drawbacks with BDG is a, drop in SO2 with exercise. Although desaturation after the, hemi-Mustard-Rastelli-BDG procedure (90.2% � 3.7) was, not statistically different with other groups, it has potential, clinical implications. The main reason for this desaturation, may be unroofed coronary sinus, where the desaturated, blood drains to the systemic circulation. Long-term results, of desaturation need to be closely followed-up., Limitations of this study included its retrospective and, single institutional design. Objective assessments of, , Downloaded for Abhishek Srivastava (sri.ab78@gmail.com) at Fortis Escorts Heart Institute and Research Centre from ClinicalKey.com by, Elsevier on November 07, 2021. For personal use only. No other uses without permission. Copyright ©2021. Elsevier Inc. All rights reserved.